Final ID: MDP1047
Trends and Sociodemographic Disparities in Cardiovascular Mortality Among People Living with HIV: A Retrospective Analysis from 1999 to 2020
Abstract Body (Do not enter title and authors here): Background:
Despite advances in treatment extending lifespans, people living with HIV (PLWH) continue to face significantly elevated risks of cardiovascular diseases (CVD). We conducted a retrospective study to investigate the current trends in CVD mortality within this demographic.
Methods:
We queried the data from the Centers for Disease Control and Prevention's Wide-ranging Online Data for Epidemiologic Research database and analyzed individuals aged 25 and above with HIV where CVD was the underlying cause of death. Age-adjusted mortality rates (AAMR) per 1 million individuals from 1999 to 2020 were calculated, along with subgroup analyses by gender, race, and region. Additionally, proportionate CVD mortality was assessed by comparing the CVD mortality to all-cause mortality among PLWH.
Results:
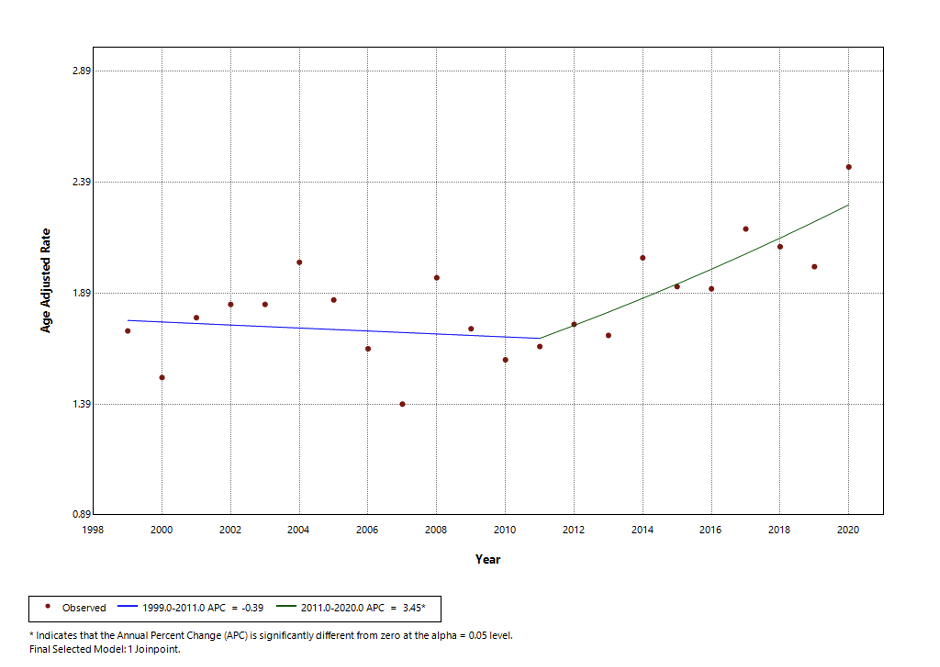
In our study, we identified 9,014 CVD mortality among PLWH. The AAMR rose from 1.72 per million (95% CI, 1.53–1.91) in 1999 to 2.46 per million (95% CI, 2.27–2.65) by 2020. A distinct gender disparity was evident; men had significantly higher AAMRs than women (3.08 vs 0.84 respectively). Racial disparities were also pronounced; Black or African American individuals exhibited a substantially higher AAMR at 8.45 (95% CI, 8.20-8.70) compared to White individuals, who had an AAMR of 1.10 (95% CI, 1.07-1.14). Regionally, the Midwest reported the lowest AAMR relative to other U.S. regions. Most notably, the proportionate CVD mortality has significantly increased from 1999 to 2020.
Conclusion:
While there has been a reduction in all-cause mortality among people living with HIV (PLWH), both absolute and proportionate cardiovascular disease (CVD) mortality rates have seen a rise, marked by significant disparities across gender, race, and regional lines. This highlights the need for further research to identify and address risk factors, particularly those extending beyond traditional cardiovascular metrics in order to improve outcomes for this vulnerable population.
Despite advances in treatment extending lifespans, people living with HIV (PLWH) continue to face significantly elevated risks of cardiovascular diseases (CVD). We conducted a retrospective study to investigate the current trends in CVD mortality within this demographic.
Methods:
We queried the data from the Centers for Disease Control and Prevention's Wide-ranging Online Data for Epidemiologic Research database and analyzed individuals aged 25 and above with HIV where CVD was the underlying cause of death. Age-adjusted mortality rates (AAMR) per 1 million individuals from 1999 to 2020 were calculated, along with subgroup analyses by gender, race, and region. Additionally, proportionate CVD mortality was assessed by comparing the CVD mortality to all-cause mortality among PLWH.
Results:
In our study, we identified 9,014 CVD mortality among PLWH. The AAMR rose from 1.72 per million (95% CI, 1.53–1.91) in 1999 to 2.46 per million (95% CI, 2.27–2.65) by 2020. A distinct gender disparity was evident; men had significantly higher AAMRs than women (3.08 vs 0.84 respectively). Racial disparities were also pronounced; Black or African American individuals exhibited a substantially higher AAMR at 8.45 (95% CI, 8.20-8.70) compared to White individuals, who had an AAMR of 1.10 (95% CI, 1.07-1.14). Regionally, the Midwest reported the lowest AAMR relative to other U.S. regions. Most notably, the proportionate CVD mortality has significantly increased from 1999 to 2020.
Conclusion:
While there has been a reduction in all-cause mortality among people living with HIV (PLWH), both absolute and proportionate cardiovascular disease (CVD) mortality rates have seen a rise, marked by significant disparities across gender, race, and regional lines. This highlights the need for further research to identify and address risk factors, particularly those extending beyond traditional cardiovascular metrics in order to improve outcomes for this vulnerable population.
More abstracts on this topic:
Acute Exposure to High PM2.5 Levels Increases the Risk of Late All-Cause Mortality in Patients with STEMI
Fathieh Sina, Tran Hao, Faour Amir, Pahn Reece, Long Mitchell, Tam Gladys, Figtree Gemma, Negishi Kazuaki, French John
10-Year Trends in Last Known Well to Arrival Time in Acute Ischemic Stroke Patients: 2014-2023Ferrone Nicholas, Sanmartin Maria, O'hara Joseph, Jimenez Jean, Ferrone Sophia, Wang Jason, Katz Jeffrey, Sanelli Pina