Final ID: MDP271
Leadless Pacemaker vs. Transvenous Pacemaker in End Stage Kidney Disease: Insights from the Nationwide Readmission Database
Abstract Body (Do not enter title and authors here): Background
Leadless pacemakers offer a safe and effective alternative pacing strategy, crucial for patients with end-stage renal disease (ESRD) overcoming vascular access isues. However, there is limited data available on their use in this population.
Methods
We utilized the Nationwide Readmission Database to extract data on all adult patients with ESRD who received either traditional transvenous or leadless pacemaker implantation from 2016 to 2021. We then compared in-hospital mortality, in-hospital complications, healthcare resource utilization, and 30-day readmission rates between these two groups.
Results
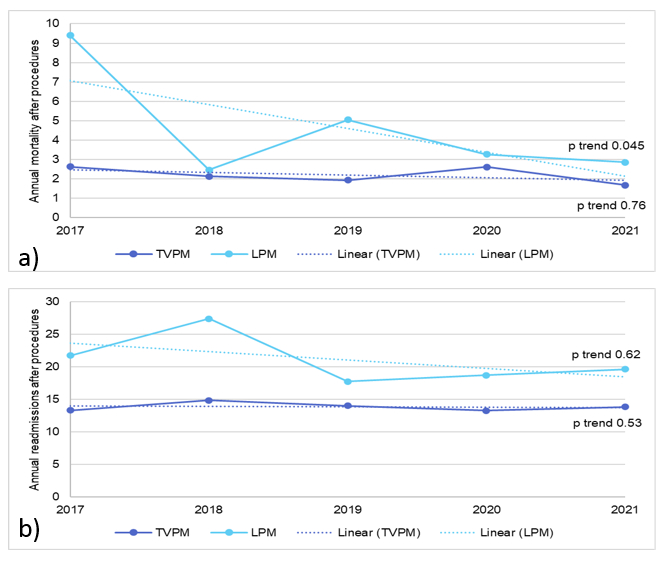
A total of 6,384 patients (81.2%) were included in the transvenous pacemaker cohort, while 1,481 patients (18.8%) were in the leadless pacemaker cohort. In ESRD patients, leadless pacemaker implantation was associated with higher in-hospital complications compared to transvenous pacemakers, including cardiac complications (aOR 4.12, CI 1.70-9.98, p<0.01), vascular complications (aOR 3.6, CI 1.40-9.26, p=0.01), and the need for blood transfusions (aOR 1.85, CI 1.32-2.60, p<0.01). There was no difference between the cohorts in terms of in-hospital mortality and 30-day readmission rates. However, the median length of stay was longer for leadless pacemaker implantation (5 days vs. 4 days, p<0.01), and the total hospitalization charges were higher ($139,826 vs. $93,919, p<0.01).
Conclusion
In conclusion, while LPM implantation in ESRD patients was associated with higher in-hospital complications and healthcare resource utilization compared to TVPM, there was no significant difference in in-hospital mortality and 30-day readmission rates. Further research is needed to understand the nature of these complications and optimize outcomes for ESRD patients undergoing LPM implantation.
Leadless pacemakers offer a safe and effective alternative pacing strategy, crucial for patients with end-stage renal disease (ESRD) overcoming vascular access isues. However, there is limited data available on their use in this population.
Methods
We utilized the Nationwide Readmission Database to extract data on all adult patients with ESRD who received either traditional transvenous or leadless pacemaker implantation from 2016 to 2021. We then compared in-hospital mortality, in-hospital complications, healthcare resource utilization, and 30-day readmission rates between these two groups.
Results
A total of 6,384 patients (81.2%) were included in the transvenous pacemaker cohort, while 1,481 patients (18.8%) were in the leadless pacemaker cohort. In ESRD patients, leadless pacemaker implantation was associated with higher in-hospital complications compared to transvenous pacemakers, including cardiac complications (aOR 4.12, CI 1.70-9.98, p<0.01), vascular complications (aOR 3.6, CI 1.40-9.26, p=0.01), and the need for blood transfusions (aOR 1.85, CI 1.32-2.60, p<0.01). There was no difference between the cohorts in terms of in-hospital mortality and 30-day readmission rates. However, the median length of stay was longer for leadless pacemaker implantation (5 days vs. 4 days, p<0.01), and the total hospitalization charges were higher ($139,826 vs. $93,919, p<0.01).
Conclusion
In conclusion, while LPM implantation in ESRD patients was associated with higher in-hospital complications and healthcare resource utilization compared to TVPM, there was no significant difference in in-hospital mortality and 30-day readmission rates. Further research is needed to understand the nature of these complications and optimize outcomes for ESRD patients undergoing LPM implantation.
More abstracts on this topic:
Brash Syndrome Requiring Permanent Pacemaker: A Case Report
Bhatt Nilay, Mrad Yves Najm, Gupta Shivam, Dickey Curtis
Age-standardized trends in Incidence Rates of Noncommunicable diseases among Adults Aged 30 to 79 in Senegal from 2000 to 2019Gaye Ngone, Ka Mame, Kyem Damaris, Jobe Modou, Sattler Elisabeth, Gary-webb Tiffany, Gaye Bamba