Final ID: MDP1381
Comparative Outcomes of Transcatheter Aortic Valve Implantation and Surgical Aortic Valve Replacement in Patients with Right Heart Failure: Insights from Nationwide Readmission Database
Abstract Body (Do not enter title and authors here): Background
The annual number of transcatheter aortic valve implantation (TAVI) performed has surpassed that of surgical aortic valve replacement (SAVR) as its use expands to patient populations not included in initial clinical trials. However, in patients with Right Heart Failure (RHF), the outcomes of TAVI and SAVR remain unclear.
Methods
We conducted a retrospective cohort study using the Nationwide Readmission Database from 2018 to 2021. Using ICD-10 codes, we identified all adult admissions for TAVI and SAVR with the presence of RHF. The primary outcome was in-hospital mortality. Secondary outcomes included in-hospital complications, 30-day readmission rate, length of stay, and total hospitalization charges.
Results
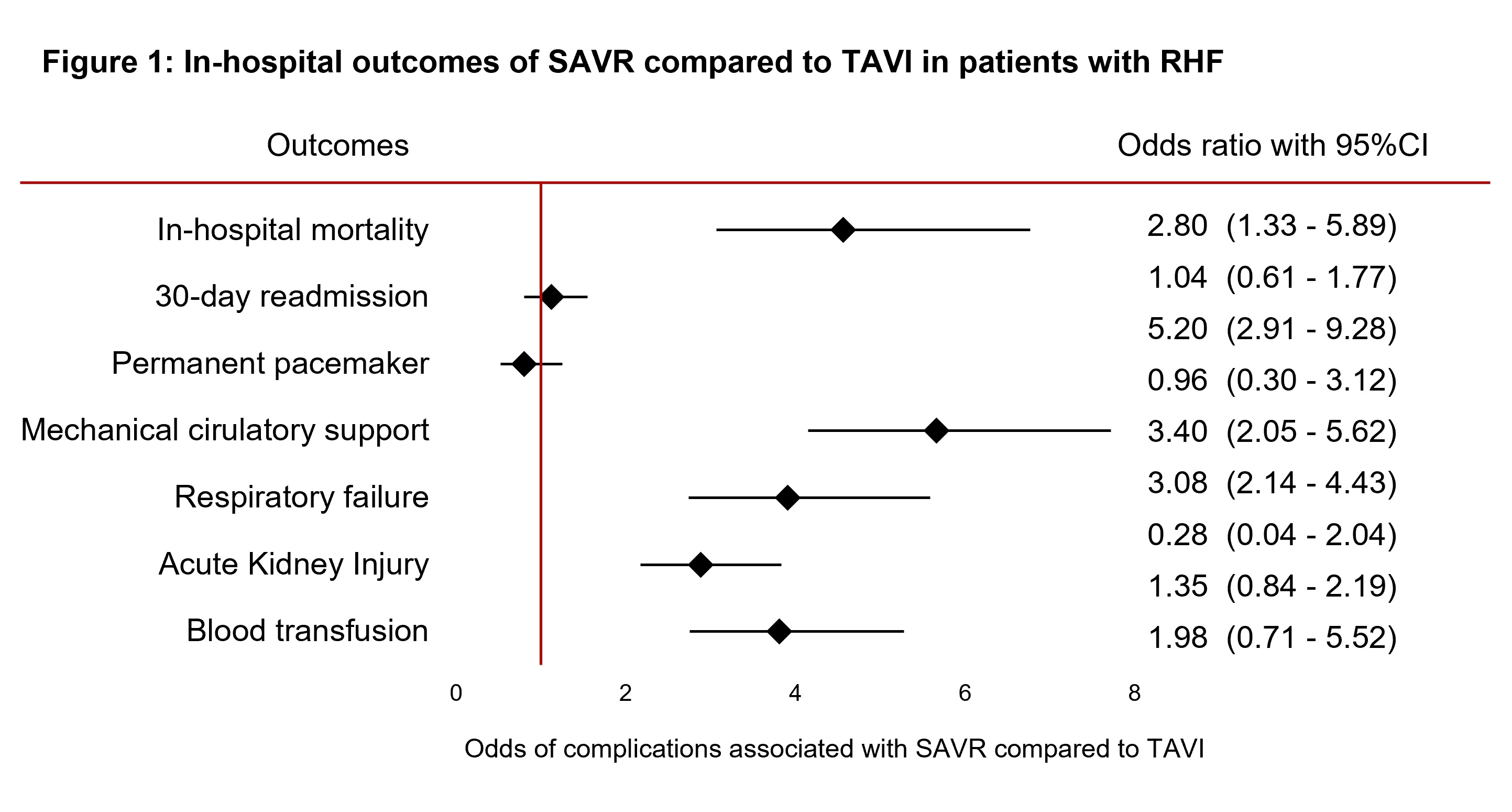
The study included 3,712 adult patients with RHF, of which 1,386 (37.3%) underwent TAVI and 2,326 (62.7%) underwent SAVR. Compared to SAVR patients, TAVI patients were older (63 years vs. 76 years, p<0.01) and had a higher burden of peripheral vascular disease, chronic liver disease, and coagulopathy, while SAVR patients had a higher burden of hypertension, diabetes mellitus, coronary artery disease, left heart failure, chronic lung disease, smoking, malignancy, and anemia. On multivariable analysis, compared to TAVI, SAVR was associated with higher odds of mortality (26.6% vs. 9.3%, p<0.01), mechanical circulatory support use (41.5% vs. 9.22%, p<0.01), respiratory failure (34.2% vs. 10.2%, p<0.01), acute kidney injury (58.1% vs. 37.7%, p<0.01), and need for blood transfusion (31.4% vs. 11.0%, p<0.01). There was no difference in 30-day readmission (13.8% vs. 14.3%, p=0.51) and permanent pacemaker implantation (7.0% vs. 8.7%, p=0.33). SAVR was associated with a longer median hospital stay (14 days vs. 8 days, p<0.01) and higher hospitalization charges ($406,826 vs $265,303, p<0.01). When compared to patients wihout RHF, the presence of RHF predicted higher in-hospital mortality for both TAVI (9.3% vs. 1.2%, p<0.01) as well as SAVR (26.6% vs. 3.7%, p<0.01).
Conclusions
From 2018 to 2021, more RHF patients underwent SAVR (62.7%) than TAVI (37.3%), but SAVR was associated with worse short-term outcomes, including higher in-hospital mortality, in-hospital complications, and healthcare resource utilization.
The annual number of transcatheter aortic valve implantation (TAVI) performed has surpassed that of surgical aortic valve replacement (SAVR) as its use expands to patient populations not included in initial clinical trials. However, in patients with Right Heart Failure (RHF), the outcomes of TAVI and SAVR remain unclear.
Methods
We conducted a retrospective cohort study using the Nationwide Readmission Database from 2018 to 2021. Using ICD-10 codes, we identified all adult admissions for TAVI and SAVR with the presence of RHF. The primary outcome was in-hospital mortality. Secondary outcomes included in-hospital complications, 30-day readmission rate, length of stay, and total hospitalization charges.
Results
The study included 3,712 adult patients with RHF, of which 1,386 (37.3%) underwent TAVI and 2,326 (62.7%) underwent SAVR. Compared to SAVR patients, TAVI patients were older (63 years vs. 76 years, p<0.01) and had a higher burden of peripheral vascular disease, chronic liver disease, and coagulopathy, while SAVR patients had a higher burden of hypertension, diabetes mellitus, coronary artery disease, left heart failure, chronic lung disease, smoking, malignancy, and anemia. On multivariable analysis, compared to TAVI, SAVR was associated with higher odds of mortality (26.6% vs. 9.3%, p<0.01), mechanical circulatory support use (41.5% vs. 9.22%, p<0.01), respiratory failure (34.2% vs. 10.2%, p<0.01), acute kidney injury (58.1% vs. 37.7%, p<0.01), and need for blood transfusion (31.4% vs. 11.0%, p<0.01). There was no difference in 30-day readmission (13.8% vs. 14.3%, p=0.51) and permanent pacemaker implantation (7.0% vs. 8.7%, p=0.33). SAVR was associated with a longer median hospital stay (14 days vs. 8 days, p<0.01) and higher hospitalization charges ($406,826 vs $265,303, p<0.01). When compared to patients wihout RHF, the presence of RHF predicted higher in-hospital mortality for both TAVI (9.3% vs. 1.2%, p<0.01) as well as SAVR (26.6% vs. 3.7%, p<0.01).
Conclusions
From 2018 to 2021, more RHF patients underwent SAVR (62.7%) than TAVI (37.3%), but SAVR was associated with worse short-term outcomes, including higher in-hospital mortality, in-hospital complications, and healthcare resource utilization.
More abstracts on this topic:
A Hard Start: Early, Intensive Healthcare Utilization for Children with Critical Congenital Heart Disease
Ellis Danielle, Hall Matthew, Blume Elizabeth, Wolfe Joanne, Snaman Jennifer, Berry Jay
A Multicenter Observational Study of Bleeding Events in Critically Ill Surgical and Trauma AdolescentsRahman Fahmid, Faustino E. Vincent, Popham Jonathan