Final ID: 4140939
Platelet-to-Lymphocyte Ratio (PLR) as a Predictor of In-Hospital Mortality in Patients with First-Ever Acute Ischemic Stroke: A cross-sectional study from Ecuador.
Abstract Body (Do not enter title and authors here): Background: In-hospital mortality from acute ischemic stroke (AIS) remains a major concern in developing countries where access to thrombectomy or fibrinolytics is limited. Platelet-to-lymphocyte ratio (PLR) has been suggested as an inflammatory marker associated with poor outcomes in AIS. Therefore, we aim to evaluate the value of PLR as a predictor of in-hospital mortality in first-ever AIS.
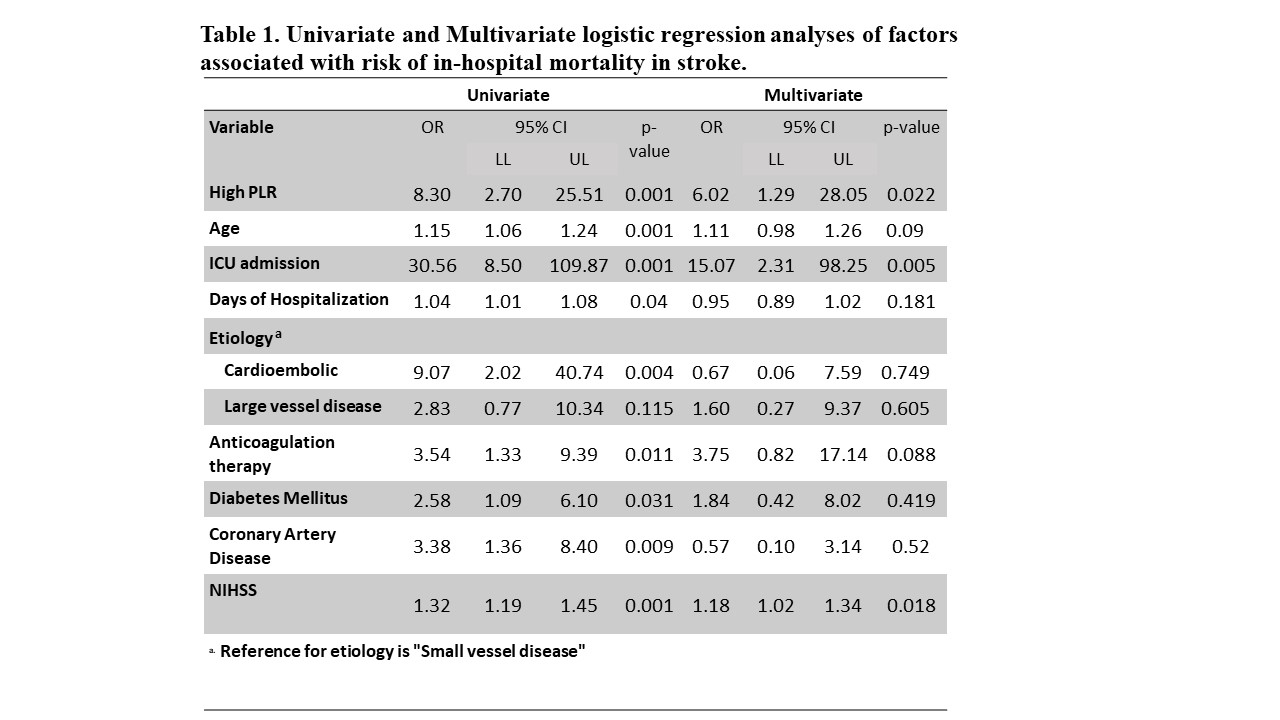
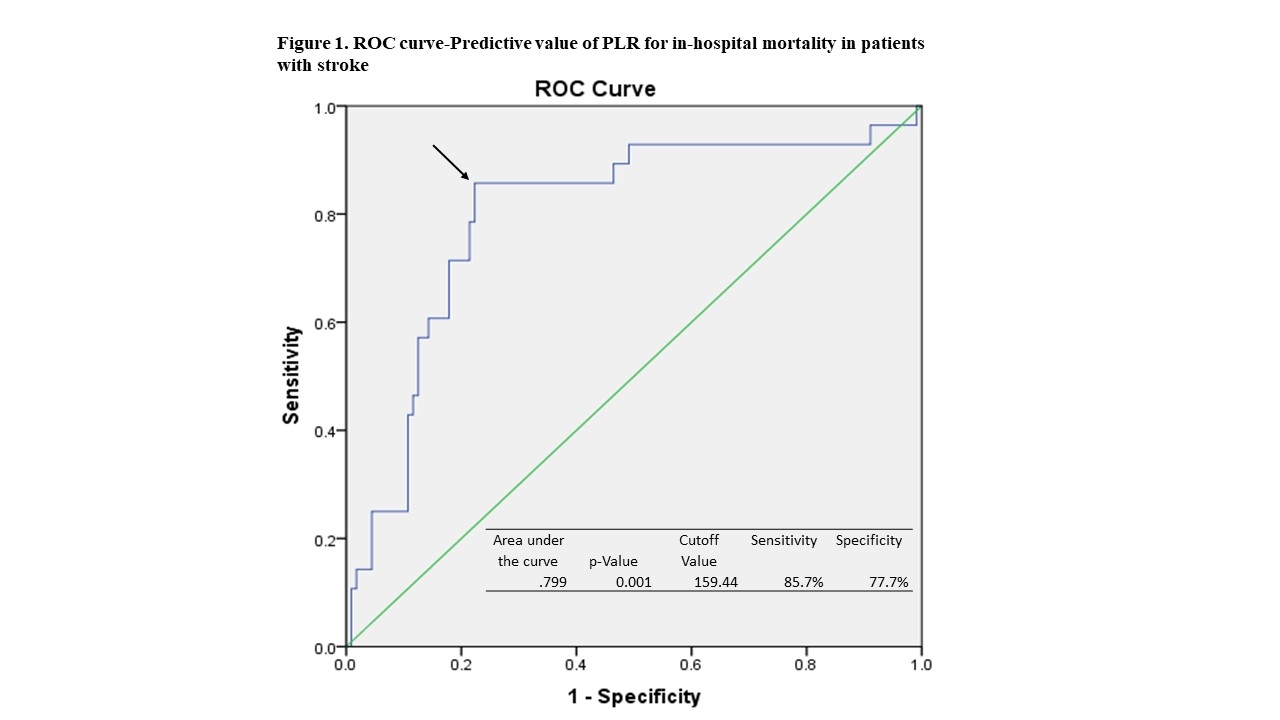
Methods: We evaluated the records of 293 patients with a first-ever AIS from a third-level hospital in Ecuador from 2016-2022. Immunocompromised patients, those who had active infections, autoimmune diseases, or malignancies were excluded. The PLR was calculated by dividing platelet by lymphocyte count. Participants were classified into low or high PLR groups based on the median. Univariate and multivariate logistic analyses were used to determine predictors of in-hospital mortality. A ROC curve analysis was performed to identify the optimal cutoff value of PLR for predicting the outcome.
Results: 140 patients were eligible for the study. Most patients were male (67.1%) and the median age was 63 years. The median length of hospitalization was 11 days (6-19), and 35% of patients required ICU admission. In-hospital mortality was 20%. Deceased patients were significantly older and had higher rates of ICU admission and NIHSS than survivors. A high PLR was associated with an increased risk of in-hospital mortality (OR =8.30; p= 0.001) in the univariate model. After adjusting for potential confounders, only high PLR (OR =6.02; p= 0.022), ICU admission, and NIHSS remained statistically significant. The ROC curve showed that the optimal cutoff value of PLR for predicting in-hospital mortality was 159.44, with an AUC of 0.799 (Sensitivity: 85.7%, Specificity:77.7%).
Conclusion: Our results suggest that PLR is an independent predictor for in-hospital mortality in patients with a first-ever AIS. This biomarker could be useful in developing countries where stroke mortality is still high.
Methods: We evaluated the records of 293 patients with a first-ever AIS from a third-level hospital in Ecuador from 2016-2022. Immunocompromised patients, those who had active infections, autoimmune diseases, or malignancies were excluded. The PLR was calculated by dividing platelet by lymphocyte count. Participants were classified into low or high PLR groups based on the median. Univariate and multivariate logistic analyses were used to determine predictors of in-hospital mortality. A ROC curve analysis was performed to identify the optimal cutoff value of PLR for predicting the outcome.
Results: 140 patients were eligible for the study. Most patients were male (67.1%) and the median age was 63 years. The median length of hospitalization was 11 days (6-19), and 35% of patients required ICU admission. In-hospital mortality was 20%. Deceased patients were significantly older and had higher rates of ICU admission and NIHSS than survivors. A high PLR was associated with an increased risk of in-hospital mortality (OR =8.30; p= 0.001) in the univariate model. After adjusting for potential confounders, only high PLR (OR =6.02; p= 0.022), ICU admission, and NIHSS remained statistically significant. The ROC curve showed that the optimal cutoff value of PLR for predicting in-hospital mortality was 159.44, with an AUC of 0.799 (Sensitivity: 85.7%, Specificity:77.7%).
Conclusion: Our results suggest that PLR is an independent predictor for in-hospital mortality in patients with a first-ever AIS. This biomarker could be useful in developing countries where stroke mortality is still high.
More abstracts on this topic:
84 Immune checkpoint profiling in major aortic diseases leads to identification of potential roles of CD155-CD206 pathway in suppressing inflammation and immune responses
Shao Ying, Saaoud Fatma, Xu Keman, Lu Yifan, Jiang Xiaohua, Wang Hong, Yang Xiaofeng
A Fecal-Derived Commensal Bacterium BM109 Reduces Infarct Size and Neurological Deficits in an Ischemic Stroke Rat ModelYoon Chung Eun, Kim You Bin, Nam Hyo Suk