Final ID: Su2136
Impact of Tricuspid Regurgitation on In-hospital Mortality in Patients with Heart Failure – United States Population-Based Survey Analysis
Abstract Body (Do not enter title and authors here): Background: Tricuspid regurgitation (TR) is a common occurrence in patients with heart failure (HF), and its role in disease progression has gained attention in recent years. While TR can worsen the clinical outcomes in HF patients, its impact on gender, racial and socioeconomic factors remains largely unexplored. With growing evidence supporting the role of percutaneous interventions for the treatment of significant TR, understanding these disparities is more crucial than ever.
Methods: Data was extracted from the National Inpatient Sample 2016 - 2020 Database. We used ICD-10 code I50 to identify the patients primarily admitted for HF and subdivided the cohort into two groups based on presence or absence of TR using the ICD-10 codes I36.1 and I07.1. We performed multivariable Logistic regression analysis to determine odds of in-hospital mortality in HF patients with and without TR. Subgroup analyses were performed based on (1) gender, (2) age, (3) race, (4) insurance status, (5) location and teaching status of admitting hospital, and (6) patients’ household neighborhood income quartile. All the analyses were adjusted for age, gender, insurance status, Charlson co-morbidity index (CCI) and hospital characteristics. STATA 16 software was used for analysis.
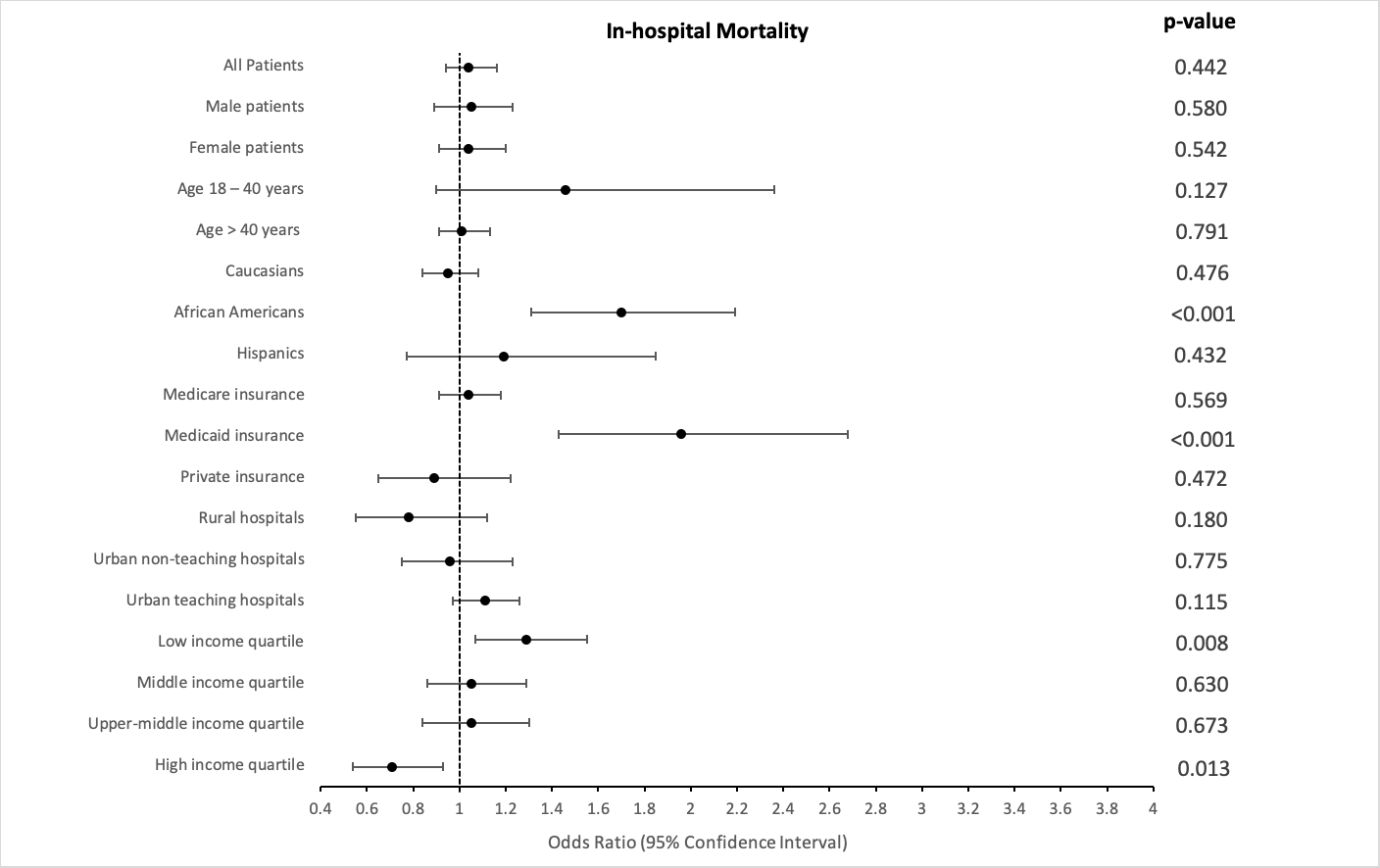
Results: Mean age of HF patients with TR was 71.3 years, mean CCI was 3.4 and 55.8% were women. In-contrast, mean age of HF patients without TR was 70.7 years, mean CCI was 3.5 and 47.5% were women. Among 1,365,529 HF patients, 41177 (3.15%) patients without TR and 1965 (3.37%) patients with TR died during the hospitalization. There was no difference in overall in-hospital mortality of HF patients with and without TR (OR: 1.04, 95% CI 0.94 – 1.16, p = 0.442). However, in subgroup analysis African Americans (OR: 1.70, 95% CI 1.31 – 2.19, p < 0.001), patients with Medicaid insurance (OR: 1.96, 95% CI 1.43 – 2.68, p < 0.001) and patients belonging to the lowest neighborhood income quartile (OR: 1.29, 95% CI 1.07 – 1.55, p = 0.008) had higher risk of in-hospital mortality as shown in Figure 1.
Conclusion: In our population-based survey analysis, we observed significant racial and socioeconomic disparities in clinical outcomes of HF patients with TR compared to those without TR. Among HF patients with TR, African Americans, patients with Medicaid insurance and patients belonging to lowest neighborhood income quartile had higher risk of in-hospital mortality compared to those without TR.
Methods: Data was extracted from the National Inpatient Sample 2016 - 2020 Database. We used ICD-10 code I50 to identify the patients primarily admitted for HF and subdivided the cohort into two groups based on presence or absence of TR using the ICD-10 codes I36.1 and I07.1. We performed multivariable Logistic regression analysis to determine odds of in-hospital mortality in HF patients with and without TR. Subgroup analyses were performed based on (1) gender, (2) age, (3) race, (4) insurance status, (5) location and teaching status of admitting hospital, and (6) patients’ household neighborhood income quartile. All the analyses were adjusted for age, gender, insurance status, Charlson co-morbidity index (CCI) and hospital characteristics. STATA 16 software was used for analysis.
Results: Mean age of HF patients with TR was 71.3 years, mean CCI was 3.4 and 55.8% were women. In-contrast, mean age of HF patients without TR was 70.7 years, mean CCI was 3.5 and 47.5% were women. Among 1,365,529 HF patients, 41177 (3.15%) patients without TR and 1965 (3.37%) patients with TR died during the hospitalization. There was no difference in overall in-hospital mortality of HF patients with and without TR (OR: 1.04, 95% CI 0.94 – 1.16, p = 0.442). However, in subgroup analysis African Americans (OR: 1.70, 95% CI 1.31 – 2.19, p < 0.001), patients with Medicaid insurance (OR: 1.96, 95% CI 1.43 – 2.68, p < 0.001) and patients belonging to the lowest neighborhood income quartile (OR: 1.29, 95% CI 1.07 – 1.55, p = 0.008) had higher risk of in-hospital mortality as shown in Figure 1.
Conclusion: In our population-based survey analysis, we observed significant racial and socioeconomic disparities in clinical outcomes of HF patients with TR compared to those without TR. Among HF patients with TR, African Americans, patients with Medicaid insurance and patients belonging to lowest neighborhood income quartile had higher risk of in-hospital mortality compared to those without TR.
More abstracts on this topic:
Aortic Valve Neocuspidization Using Autologous Insertion Of Pulmonary SinusTm: A Proof Of Concept
Faateh Muhammad, Raees Muhammad Aanish, Ahmed Hosam, Almiqlash Bushray, Villalobos Lizardi Jose, Ricci Marco, Ashfaq Awais
A Case Presentation of Severe Left Ventricular Dysfunction from Focal Myocarditis due to Immune Checkpoint InhibitorPatel Romil, Hussain Kifah, Gordon Robert