Final ID: Su1059
Impact of Tricuspid Regurgitation on Readmission Outcomes in Patients with Heart Failure – United States Population-Based Survey Analysis
Abstract Body (Do not enter title and authors here): Background: Tricuspid regurgitation (TR) is a common occurrence in patients with heart failure (HF), and its role in disease progression has gained attention in recent years. While TR can worsen the clinical outcomes in HF patients, its impact on gender, racial and socioeconomic factors remains largely unexplored. With growing evidence supporting the role of percutaneous interventions for the treatment of significant TR, understanding these disparities is more crucial than ever.
Methods: Data was extracted from the National Readmission 2016 - 2020 Database. We used ICD-10 code I50 to identify the patients primarily admitted for HF and subdivided the cohort into two groups based on presence or absence of TR using the ICD-10 codes I36.1 and I07.1. We performed multivariable Poisson regression analysis to determine hazard ratio of 90-day HF-specific readmission in HF patients with and without TR. Subgroup analyses were performed based on (1) gender, (2) age, (3) insurance status, (4) location and teaching status of admitting hospital, and (5) patients’ household neighborhood income quartile. All the analyses were adjusted for age, gender, insurance status, Charlson co-morbidity index and hospital characteristics. STATA 16 software was used for the analysis.
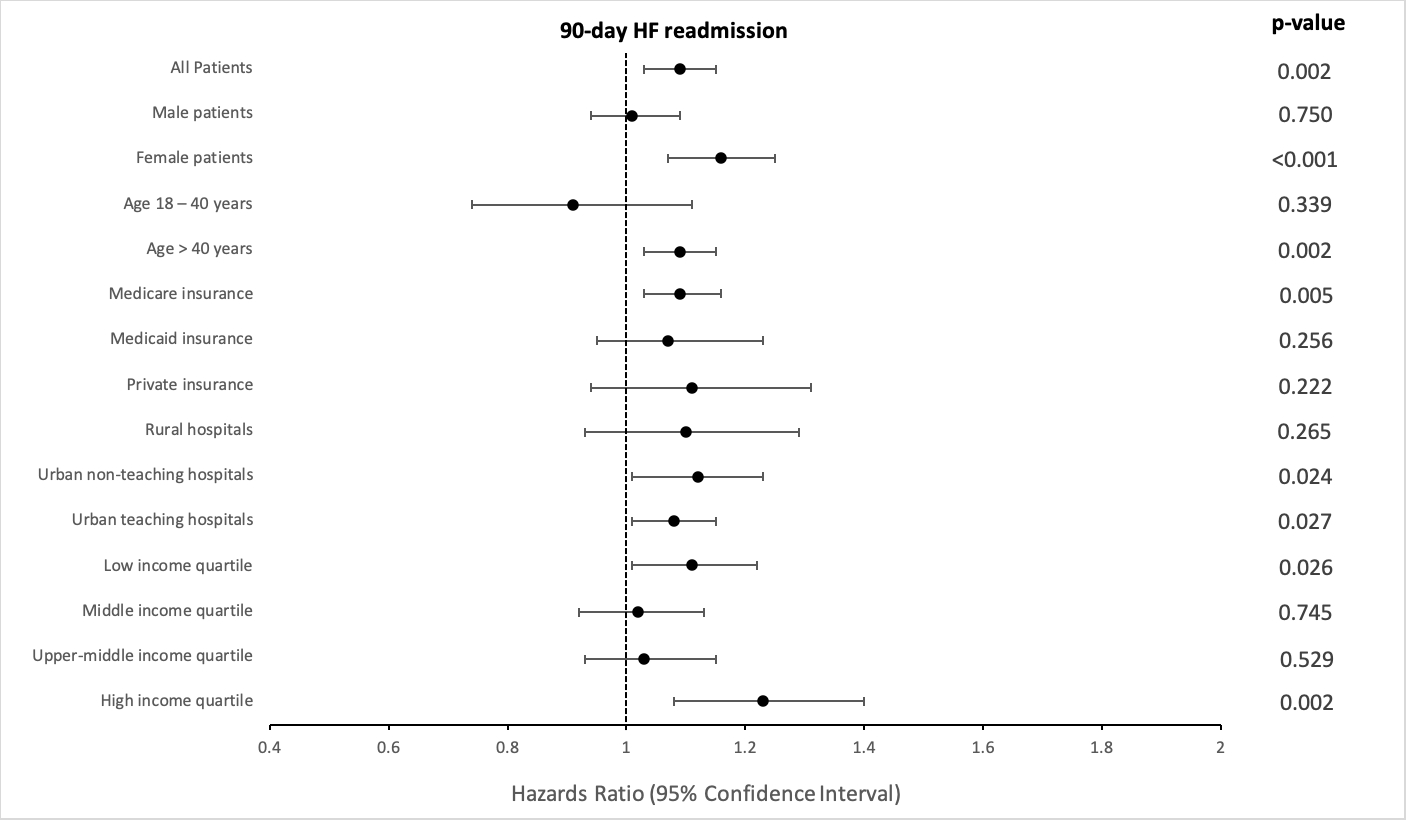
Results: Among 971,368 HF patients, 83987 (9.03%) patients without TR and 3988 (9.66%) patients with TR had a 90-day HF-specific readmission. HF patients with TR were 9% more likely to have HF-specific readmission in 90-days (HR: 1.09, 95% CI 1.03 – 1.15, p = 0.002). In the subgroup analysis, female patients (HR: 1.16, 95% CI 1.07 – 1.25, p < 0.001), patients with age > 40 years of age (HR: 1.09, 95% CI 1.03 – 1.15, p = 0.002), patients with Medicare insurance (HR: 1.09, 95% CI 1.03 – 1.16, p = 0.005), patients admitted to urban non-teaching (HR: 1.12, 95% CI 1.01 – 1.23, p = 0.024) and urban teaching hospitals (HR: 1.08, 95% CI 1.01 – 1.15, p = 0.027) and the patients belonging to the lowest (HR: 1.11, 95% CI 1.01 – 1.22, p = 0.026) and the highest household neighborhood income quartiles (HR: 1.23, 95% CI 1.08 – 1.40, p = 0.002) had higher risk of 90-day HF-specific readmission as shown in Figure 1.
Conclusion: In our adjusted population-based survey analysis, we observed significant gender, socioeconomic and hospital-based disparities in readmission outcomes of HF patients with TR compared to those without TR.
Methods: Data was extracted from the National Readmission 2016 - 2020 Database. We used ICD-10 code I50 to identify the patients primarily admitted for HF and subdivided the cohort into two groups based on presence or absence of TR using the ICD-10 codes I36.1 and I07.1. We performed multivariable Poisson regression analysis to determine hazard ratio of 90-day HF-specific readmission in HF patients with and without TR. Subgroup analyses were performed based on (1) gender, (2) age, (3) insurance status, (4) location and teaching status of admitting hospital, and (5) patients’ household neighborhood income quartile. All the analyses were adjusted for age, gender, insurance status, Charlson co-morbidity index and hospital characteristics. STATA 16 software was used for the analysis.
Results: Among 971,368 HF patients, 83987 (9.03%) patients without TR and 3988 (9.66%) patients with TR had a 90-day HF-specific readmission. HF patients with TR were 9% more likely to have HF-specific readmission in 90-days (HR: 1.09, 95% CI 1.03 – 1.15, p = 0.002). In the subgroup analysis, female patients (HR: 1.16, 95% CI 1.07 – 1.25, p < 0.001), patients with age > 40 years of age (HR: 1.09, 95% CI 1.03 – 1.15, p = 0.002), patients with Medicare insurance (HR: 1.09, 95% CI 1.03 – 1.16, p = 0.005), patients admitted to urban non-teaching (HR: 1.12, 95% CI 1.01 – 1.23, p = 0.024) and urban teaching hospitals (HR: 1.08, 95% CI 1.01 – 1.15, p = 0.027) and the patients belonging to the lowest (HR: 1.11, 95% CI 1.01 – 1.22, p = 0.026) and the highest household neighborhood income quartiles (HR: 1.23, 95% CI 1.08 – 1.40, p = 0.002) had higher risk of 90-day HF-specific readmission as shown in Figure 1.
Conclusion: In our adjusted population-based survey analysis, we observed significant gender, socioeconomic and hospital-based disparities in readmission outcomes of HF patients with TR compared to those without TR.
More abstracts on this topic:
Chronic Kidney Disease is Associated With Decreased Survival In Patients with Cardiogenic Shock and Tricuspid Regurgitation
Ramchandani Sunil, Oren Daniel, Nair Ranjit, Szinte Julia, Lorenzana Adrian, Pink Kevin, Zepeda Ignacio
A Novel Composite Artificial Intelligence-Electrocardiography Risk Score Is Independently Associated with Mortality in Chronic Tricuspid RegurgitationCiobanu Andrea, Pellikka Patricia, Kane Garvan, Pislaru Sorin, Anand Vidhu, Naser Jwan, Wood Julia, Friedman Paul, Vinereanu Dragos, Nkomo Vuyisile, Pislaru Cristina, Lara-breitinger Kyla, Thaden Jeremy