Final ID: MDP1523
Prevalence, Clinical Correlates, and Outcomes of Tricuspid Regurgitation Among Older Adults: The Atherosclerosis Risk in Communities Study
Abstract Body (Do not enter title and authors here): Introduction: Tricuspid regurgitation (TR) prevalence increases with age and is associated with higher mortality. Limited data exist regarding the prognostic relevance of TR among older adults in the general population.
Objective: To estimate the prevalence of TR in late life, identify cardiac structural and functional measures associated with TR severity, and determine the prognostic relevance of TR severity.
Methods: In the community-based Atherosclerosis Risk in Communities (ARIC) study, 3,046 participants underwent protocol echocardiography at the 7th study visit (2018-2019). TR severity was assessed qualitatively as none/trace, mild, moderate, or severe by a board-certified cardiologist. Dyspnea was assessed using the modified Medical Research Council questionnaire and post-Visit 7 mortality was ascertained through the National Death Index. Cross-sectional associations of TR severity with clinical characteristics, echocardiographic measures, and dyspnea were assessed using multivariable linear and logistic regression models. Associations with death were assessed using Cox proportional hazard models adjusted for demographics.
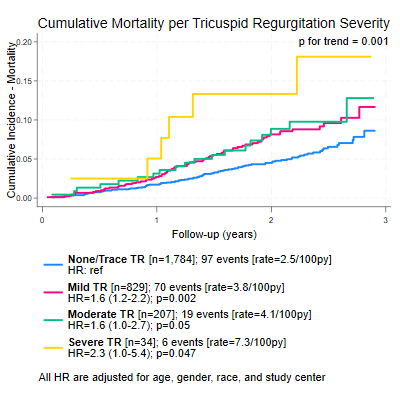
Results: Mean age was 81±4 years, 58% were women, 25% reported Black race, and mean LVEF was 63±8%. TR prevalence was 30% mild, 9% moderate, and 1% severe. Greater TR severity was associated with older age, female sex, higher HF prevalence, and loop diuretic use. Greater TR severity was also associated with lower LVEF, worse LV diastolic function (higher LAVi, E/A, E/e’ septal), higher NT-proBNP, higher prevalence of moderate-severe mitral regurgitation, greater pulmonary artery systolic pressure, and larger RV size. Severe TR was associated with higher odds of moderate-severe dyspnea (OR:2.3 [1.2-4.5], p=0.012). During follow-up (median 2.1 years [IQR 1.7-2.5]), 192 participants died. Higher TR severity was associated with greater mortality (Figure). Compared to participants with none/trace TR, even mild TR was associated with a 64% greater mortality risk.
Conclusion: TR is common in late life and is associated with greater left heart disease despite generally preserved LVEF. Greater TR severity, even when mild, is a marker of increased mortality. Longer follow-up is needed to determine whether this risk is independent of concomitant left heart dysfunction.
Objective: To estimate the prevalence of TR in late life, identify cardiac structural and functional measures associated with TR severity, and determine the prognostic relevance of TR severity.
Methods: In the community-based Atherosclerosis Risk in Communities (ARIC) study, 3,046 participants underwent protocol echocardiography at the 7th study visit (2018-2019). TR severity was assessed qualitatively as none/trace, mild, moderate, or severe by a board-certified cardiologist. Dyspnea was assessed using the modified Medical Research Council questionnaire and post-Visit 7 mortality was ascertained through the National Death Index. Cross-sectional associations of TR severity with clinical characteristics, echocardiographic measures, and dyspnea were assessed using multivariable linear and logistic regression models. Associations with death were assessed using Cox proportional hazard models adjusted for demographics.
Results: Mean age was 81±4 years, 58% were women, 25% reported Black race, and mean LVEF was 63±8%. TR prevalence was 30% mild, 9% moderate, and 1% severe. Greater TR severity was associated with older age, female sex, higher HF prevalence, and loop diuretic use. Greater TR severity was also associated with lower LVEF, worse LV diastolic function (higher LAVi, E/A, E/e’ septal), higher NT-proBNP, higher prevalence of moderate-severe mitral regurgitation, greater pulmonary artery systolic pressure, and larger RV size. Severe TR was associated with higher odds of moderate-severe dyspnea (OR:2.3 [1.2-4.5], p=0.012). During follow-up (median 2.1 years [IQR 1.7-2.5]), 192 participants died. Higher TR severity was associated with greater mortality (Figure). Compared to participants with none/trace TR, even mild TR was associated with a 64% greater mortality risk.
Conclusion: TR is common in late life and is associated with greater left heart disease despite generally preserved LVEF. Greater TR severity, even when mild, is a marker of increased mortality. Longer follow-up is needed to determine whether this risk is independent of concomitant left heart dysfunction.
More abstracts on this topic:
A Hemodynamic Warning Sign: Continuous Mitral Regurgitation and Normal Sinus Rhythm
Mahi Ishani, Chowdhury Mahdi, Madan Hritik, Garg Vaani
Early Safety Signals and Common Pitfalls of the TriClip™ System for Transcatheter Tricuspid Valve Repair: Analysis of FDA's MAUDE DatabaseGupta Lovish, Gulati Arvind, Futela Pragyat, Khanna Tejasvini, Aneja Ashish, Kowlgi Gurukripa, Gupta Tanush, Chatterjee Arka