Final ID: Su4126
Non-ischemic septal fibrosis on delayed enhancement CMR provides incremental prognostic value in functional tricuspid regurgitation
Abstract Body (Do not enter title and authors here): Introduction: CMR enables assessment of cardiac chamber remodeling and associated alterations in myocardial tissue substrate. Primary aim of this study was to examine the relative prognostic utility of chamber remodeling and myocardial tissue alterations in patients with functional tricuspid regurgitation.
Methods: The population comprised patients with advanced functional TR (≥moderate) undergoing CMR. LGE-CMR was used to identify myocardial scar/infarction inclusive of non-ischemic septal fibrosis (NIsF) which was defined as hyperenhancement in the mid-myocardial or epicardial aspect of the interventricular septum. Clinical characteristics including follow-up and all-cause mortality were obtained blinded to imaging analyses.
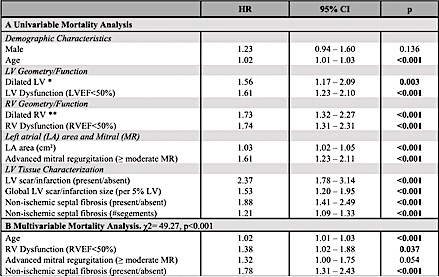
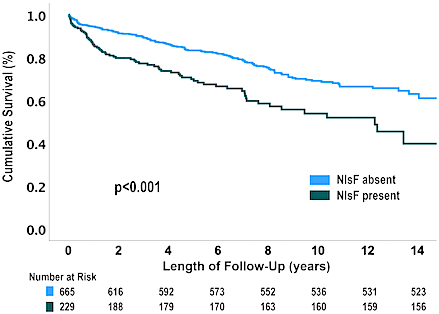
Results: 894 pts (71±15yo; 52% male) with advanced functional TR undergoing CMR were studied; LV dysfunction was present in 44% and RV dysfunction in 57%. Paralleling ventricular dysfunction, adverse LV and RV chamber remodeling was also common, occuring in 25% and 43% of the population, respectively. Regarding tissue substrate, over half (50.4%) had LV scar/infarction (9.2±10.8 %LV), 50.8% of which represented NIsF. Prevalence of NIsF was 3-fold higher in patients with concomitant RV dysfunction versus those without (36.1% vs 11.5%, p<0.001). Regarding outcomes, 215 patients died during a median follow-up of 4.6 years. As shown in Table 1, LV and RV dysfunction, LV and RV dilation, advanced mitral regurgitation and NIsF were each linked to increased mortality risk (all p<0.001). A combined model incorporating indices known to impact TR prognosis demonstrates NIsF to be independently linked to increased mortality risk even after controlling for RV dysfunction (HR 1.78 [CI 1.31-2.43]; p<0.001). Kaplan-Meier analysis demonstrates significantly increased risk of death in patients with NIsF (p<0.001) (Figure 1).
Conclusions: Among patients with advanced TR, NIsF provides incremental prognostic risk stratification beyond conventional risk markers.
Methods: The population comprised patients with advanced functional TR (≥moderate) undergoing CMR. LGE-CMR was used to identify myocardial scar/infarction inclusive of non-ischemic septal fibrosis (NIsF) which was defined as hyperenhancement in the mid-myocardial or epicardial aspect of the interventricular septum. Clinical characteristics including follow-up and all-cause mortality were obtained blinded to imaging analyses.
Results: 894 pts (71±15yo; 52% male) with advanced functional TR undergoing CMR were studied; LV dysfunction was present in 44% and RV dysfunction in 57%. Paralleling ventricular dysfunction, adverse LV and RV chamber remodeling was also common, occuring in 25% and 43% of the population, respectively. Regarding tissue substrate, over half (50.4%) had LV scar/infarction (9.2±10.8 %LV), 50.8% of which represented NIsF. Prevalence of NIsF was 3-fold higher in patients with concomitant RV dysfunction versus those without (36.1% vs 11.5%, p<0.001). Regarding outcomes, 215 patients died during a median follow-up of 4.6 years. As shown in Table 1, LV and RV dysfunction, LV and RV dilation, advanced mitral regurgitation and NIsF were each linked to increased mortality risk (all p<0.001). A combined model incorporating indices known to impact TR prognosis demonstrates NIsF to be independently linked to increased mortality risk even after controlling for RV dysfunction (HR 1.78 [CI 1.31-2.43]; p<0.001). Kaplan-Meier analysis demonstrates significantly increased risk of death in patients with NIsF (p<0.001) (Figure 1).
Conclusions: Among patients with advanced TR, NIsF provides incremental prognostic risk stratification beyond conventional risk markers.
More abstracts on this topic:
Burden of Non-Rheumatic Valvular Heart Disease in High-income Asia Pacific from 1990-2019: A Benchmarking analysis
Shaikh Salomi, Amin Vishrant, Desai Hardik, Sharma Kamal, Shandilya Ashwinikumar, Patel Khushbu, Waqas Muhammad, Syed Saif, Lakkimsetti Mohit, Bhalodia Paritaben, Islam Hamza, Patel Juhi
Association of Moderate-Severe Tricuspid Regurgitation with Exercise Hemodynamics and Outcomes in Patients in Heart Failure with Preserved Ejection Fraction: Multicenter StudyDorsey Natalie, Caravita Sergio, Tedford Ryan, Rao Vishal N., Baratto Claudia, Biscopink Alec, Taylor Eric, Atkins Jessica, Amoroso Nicholas, Carnicelli Anthony, Houston Brian, Silkowski Molly