Final ID: 4140082
Mediation of Higher Coronary Heart Disease Risk in Non-White Populations by Lifestyle-Psychosocial and Genetic Factors: A Comparative Analysis
Abstract Body (Do not enter title and authors here): Background: Coronary heart disease (CHD) results from environmental and genetic factors. Lifestyle-psychosocial factors that capture environmental risk and polygenic risk scores (PRS) that capture genetic risk have been associated with CHD in prior studies.
Aim: To assess whether higher CHD risk traditionally attributed to non-White race/ethnicty is mediated by PSSCHD or PRSCHD.
Methods: In UK Biobank, we ascertained incident CHD (MI/coronary revascularization) and calculated an ancestry-specific PRS for CHD (PGS000018). Based on self-reported race/ethnicity, participants were classified as White and non-White. An age, sex, and ethnicity-adjusted polysocial score for CHD (PSSCHD) was derived from 100 self-reported lifestyle-psychosocial factors across nine domains: Adulthood Relationship, Education, Entertainment, Housing, Income, Occupation, Physical Activity, Psychological Health, and Sleep. Those with CHD or statin use at recruitment or missing age, sex, race/ethnicity or genotype were excluded. Machine learning (elastic net model) was used to develop PSSCHD. Cox and mediation analyses were performed.
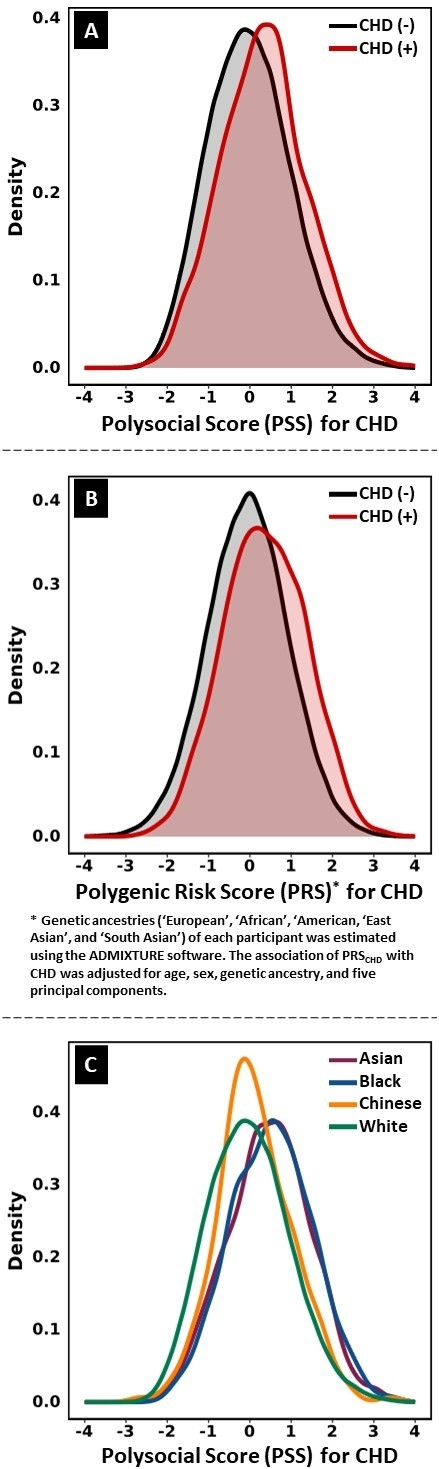
Results: In 398,403 participants (56±8 y, 43% male, 96.3% White, 1.8% Asian, 1.6% Black, and 0.3% Chinese), 10,033 had an incident CHD event during a 10-year follow-up. The HRs (95% CIs) for a 1 SD increase in PSSCHD and PRSCHD for CHD risk were 1.5 (1.4–1.5, P<10-16), and 1.6 (1.5 - 1.6, P<10-16), respectively (Figure 1A-B). Asians and Blacks had the highest PSSCHD (mean±SD: 0.5±1, and 0.5±1, respectively), followed by Chinese (0.1±0.9), and Whites (0.0±1) (Figure 1C). After adjustment for age, sex, diabetes, hypertension, LDL-C, and smoking, non-Whites had higher CHD risk: HR (95% CI): 1.2 (1.0–1.4, P<10-16), and the higher risk was mediated more substantially by PSSCHD than PRSCHD (63% (38%-100%) vs. 16% (8%-41%), both P<10-16).
Conclusions: The higher CHD risk observed in non-Whites in UK Biobank was mainly due to unfavorable lifestyle-psychosocial factors, rather than PRS, consistent with the paradigm that race/ethnicity is not a biological but rather a social construct. Our findings support substituting race/ethnicity with lifestyle-psychosocial factors and social determinants of health in CHD risk equations.
Aim: To assess whether higher CHD risk traditionally attributed to non-White race/ethnicty is mediated by PSSCHD or PRSCHD.
Methods: In UK Biobank, we ascertained incident CHD (MI/coronary revascularization) and calculated an ancestry-specific PRS for CHD (PGS000018). Based on self-reported race/ethnicity, participants were classified as White and non-White. An age, sex, and ethnicity-adjusted polysocial score for CHD (PSSCHD) was derived from 100 self-reported lifestyle-psychosocial factors across nine domains: Adulthood Relationship, Education, Entertainment, Housing, Income, Occupation, Physical Activity, Psychological Health, and Sleep. Those with CHD or statin use at recruitment or missing age, sex, race/ethnicity or genotype were excluded. Machine learning (elastic net model) was used to develop PSSCHD. Cox and mediation analyses were performed.
Results: In 398,403 participants (56±8 y, 43% male, 96.3% White, 1.8% Asian, 1.6% Black, and 0.3% Chinese), 10,033 had an incident CHD event during a 10-year follow-up. The HRs (95% CIs) for a 1 SD increase in PSSCHD and PRSCHD for CHD risk were 1.5 (1.4–1.5, P<10-16), and 1.6 (1.5 - 1.6, P<10-16), respectively (Figure 1A-B). Asians and Blacks had the highest PSSCHD (mean±SD: 0.5±1, and 0.5±1, respectively), followed by Chinese (0.1±0.9), and Whites (0.0±1) (Figure 1C). After adjustment for age, sex, diabetes, hypertension, LDL-C, and smoking, non-Whites had higher CHD risk: HR (95% CI): 1.2 (1.0–1.4, P<10-16), and the higher risk was mediated more substantially by PSSCHD than PRSCHD (63% (38%-100%) vs. 16% (8%-41%), both P<10-16).
Conclusions: The higher CHD risk observed in non-Whites in UK Biobank was mainly due to unfavorable lifestyle-psychosocial factors, rather than PRS, consistent with the paradigm that race/ethnicity is not a biological but rather a social construct. Our findings support substituting race/ethnicity with lifestyle-psychosocial factors and social determinants of health in CHD risk equations.
More abstracts on this topic:
Association of Body Size and Shape Metrics with Atherosclerotic Cardiovascular Disease and Mortality: Ethnic Differences in a Nationally Representative Cohort of U.S. Adults
Mangalesh Sridhar, Shah Priyansh, Chi Kuan Yu, Nouri Armin, Rossi Raiza, Borkowski Pawel, Faillace Robert, Nanna Michael
A Case of Transient Cortical Blindness occurring during Percutaneous Transluminal Coronary Angiography for Acute Coronary Syndrome.Adelakun Adeniyi, Farouji Iyad, Haddad Ahmad, Szwed Stanley