Final ID: Sa4086
Racial/Ethnic Disparities in Outcomes of Post-Transcatheter Aortic Valve Replacement: A Systematic Review and Meta-Analysis
Abstract Body (Do not enter title and authors here): Background:
There has been growing awareness and recognition of discrepant health outcomes based on ethnic and racial background in patients undergoing cardiovascular procedures. Transcatheter aortic valve procedures has become the primary treatment for aortic stenosis and is currently the standard of care. Despite widespread adoption of TAVR, African Americans (AA) have continued to remain underrepresented and typically suffer poorer outcomes. Thus, we conducted a systematic review and meta-analysis to compare TAVR outcomes between AA and non-AA populations.
Methodology: We systematically searched all electronic databases (PubMed, EMBASE, Scopus, Web of science) from inception until May 25th, 2024. A pooled analysis of data from observational studies and randomized controlled trials reporting post-TAVR outcomes based on racial background were included. The key endpoints evaluated were in-hospital mortality, post-procedure myocardial infarction (MI), pacemaker placement, in-hospital stroke, vascular complications, major bleeding, acute kidney injury (AKI). We used the I2 statistic to assess heterogeneity among studies using the Random-Effects model, with significance set at I2 > 50%. All analysis was carried out using R version 4.3.2.
Results:
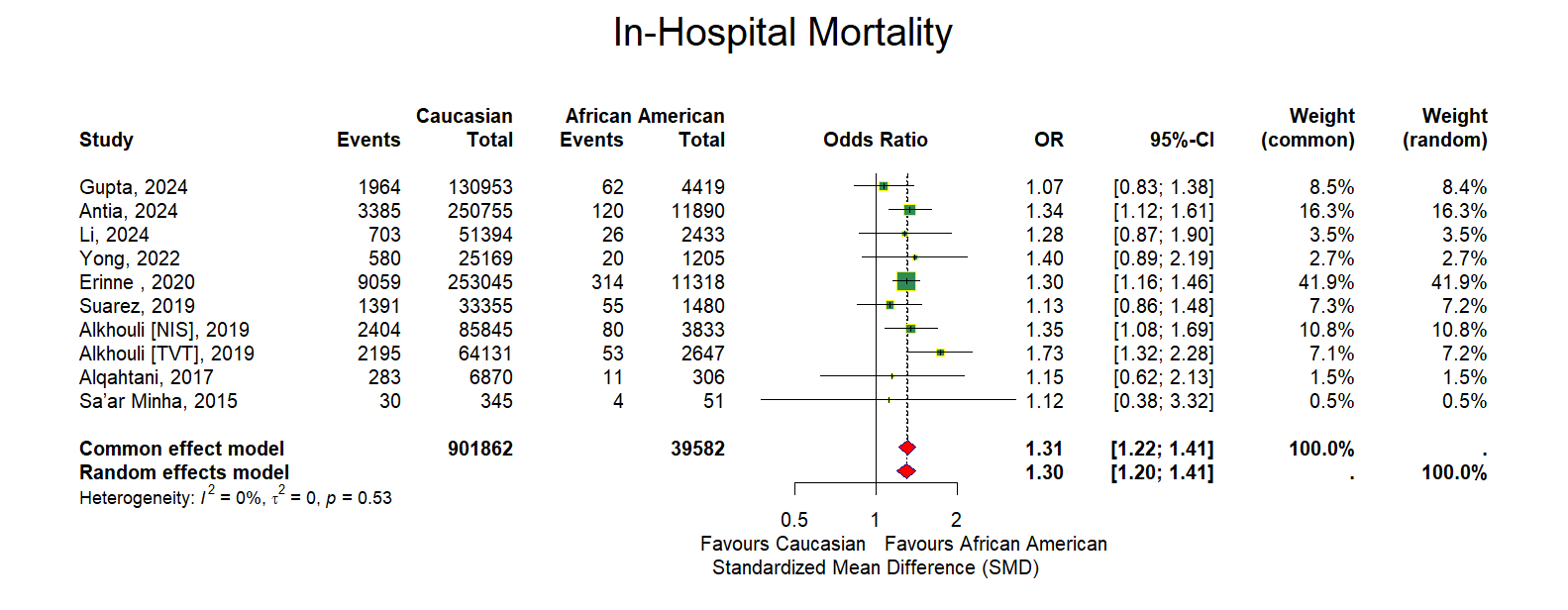
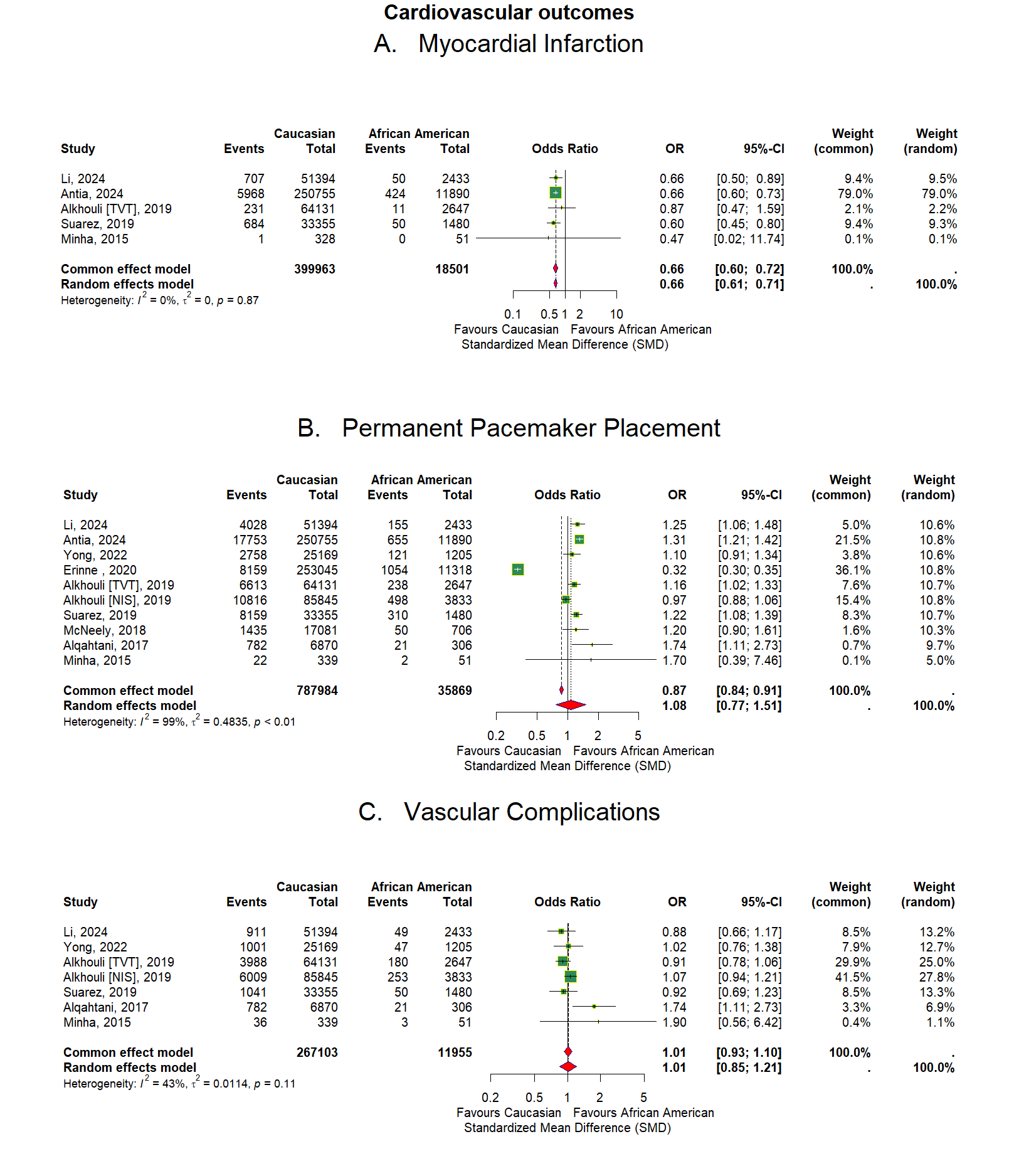
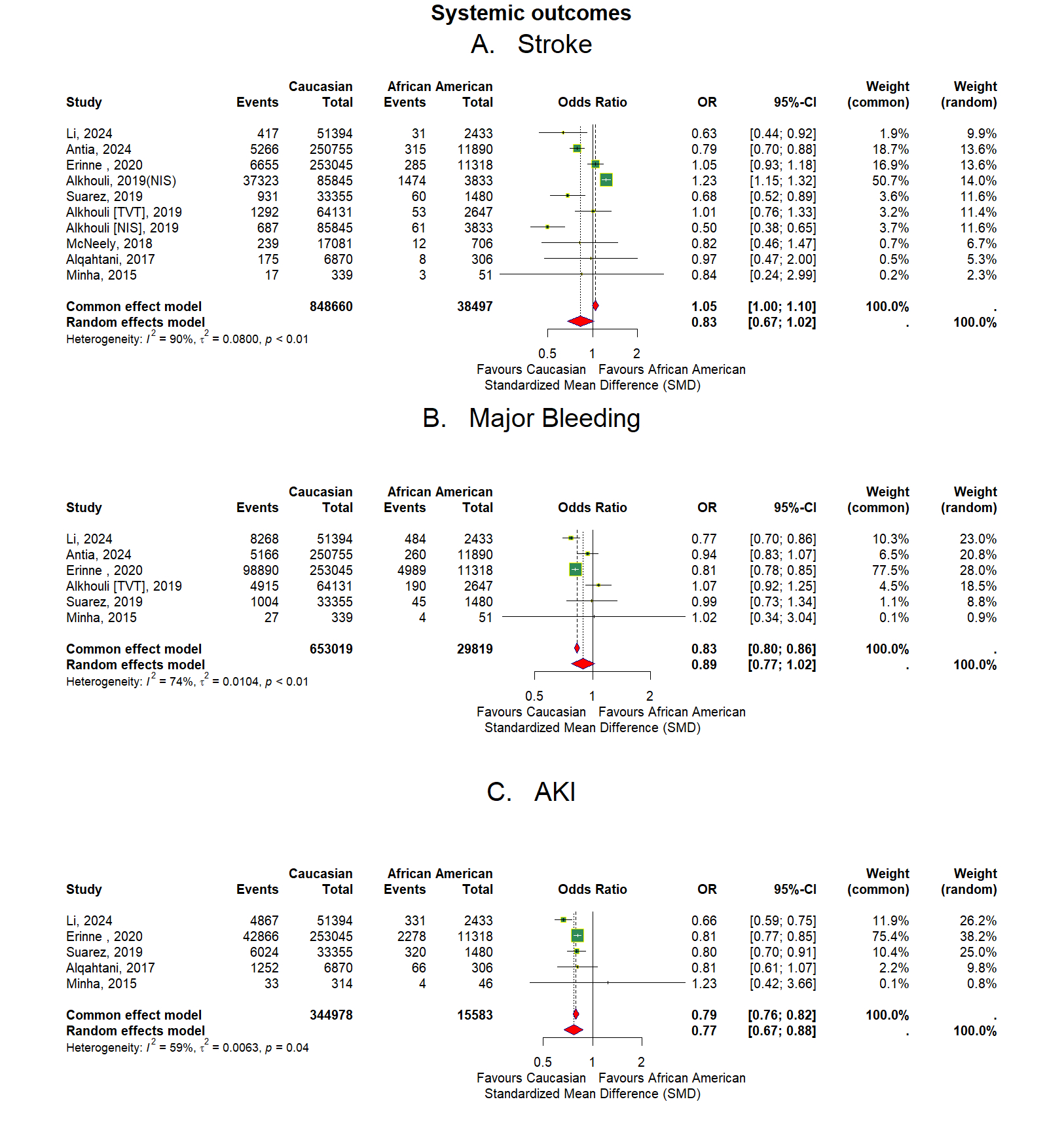
The meta-analysis of eleven observational studies, involving 953,892 TAVR patients [912,301 (95.64%) Caucasians and 41,591 (4.36%) AAs], showed a statistically significant higher risk of post-procedure pacemaker placement (OR 1.08, 95% CI: 0.77-1.51, p=<0.001, I2=99%) for Caucasians compared to AAs. In secondary outcomes, AAs had significant higher risk of in-hospital stroke (OR 0.83, 95% CI: 0.67-1.02, p <0.01, I2=90%), major bleeding (OR:0.89, 95% CI: 0.77-1.02, p <0.01, I2=74%), AKI (OR: 0.77, 95%CI:0.67-0.88, P=0.04, I2=59%) compared to Caucasians. However, no significant differences were found for in-hospital mortality, MI, vascular complications as mentioned in Figure 1-3.
Conclusion: The current study suggests a worse clinical outcome for AA undergoing TAVR. Further studies are needed to evaluate the factors responsible for the discrepancy and implementing mitigation strategies.
There has been growing awareness and recognition of discrepant health outcomes based on ethnic and racial background in patients undergoing cardiovascular procedures. Transcatheter aortic valve procedures has become the primary treatment for aortic stenosis and is currently the standard of care. Despite widespread adoption of TAVR, African Americans (AA) have continued to remain underrepresented and typically suffer poorer outcomes. Thus, we conducted a systematic review and meta-analysis to compare TAVR outcomes between AA and non-AA populations.
Methodology: We systematically searched all electronic databases (PubMed, EMBASE, Scopus, Web of science) from inception until May 25th, 2024. A pooled analysis of data from observational studies and randomized controlled trials reporting post-TAVR outcomes based on racial background were included. The key endpoints evaluated were in-hospital mortality, post-procedure myocardial infarction (MI), pacemaker placement, in-hospital stroke, vascular complications, major bleeding, acute kidney injury (AKI). We used the I2 statistic to assess heterogeneity among studies using the Random-Effects model, with significance set at I2 > 50%. All analysis was carried out using R version 4.3.2.
Results:
The meta-analysis of eleven observational studies, involving 953,892 TAVR patients [912,301 (95.64%) Caucasians and 41,591 (4.36%) AAs], showed a statistically significant higher risk of post-procedure pacemaker placement (OR 1.08, 95% CI: 0.77-1.51, p=<0.001, I2=99%) for Caucasians compared to AAs. In secondary outcomes, AAs had significant higher risk of in-hospital stroke (OR 0.83, 95% CI: 0.67-1.02, p <0.01, I2=90%), major bleeding (OR:0.89, 95% CI: 0.77-1.02, p <0.01, I2=74%), AKI (OR: 0.77, 95%CI:0.67-0.88, P=0.04, I2=59%) compared to Caucasians. However, no significant differences were found for in-hospital mortality, MI, vascular complications as mentioned in Figure 1-3.
Conclusion: The current study suggests a worse clinical outcome for AA undergoing TAVR. Further studies are needed to evaluate the factors responsible for the discrepancy and implementing mitigation strategies.
More abstracts on this topic:
APOL1 Risk Variants and Risk of Incident Atrial Fibrillation in Systolic Blood Pressure Intervention Trial (SPRINT)
Ahmad Muhammad, Kazibwe Richard, Mostafa Mohamed, Naeem Rimsha, Singh Sanjay, Bansal Nisha, Soliman Elsayed
A Randomized Clinical Trial for Asymptomatic Elevated Blood Pressure in Patients Discharged from Emergency DepartmentPrendergast Heather, Khosla Shaveta, Kitsiou Spyros, Petzel Gimbar Renee, Freels Sally, Sanders Anissa, Daviglus Martha, Carter Barry, Del Rios Marina, Heinert Sara