Final ID: Mo4130
The Hidden Killer in Patients with Sepsis Spectra Disorders: Systolic Heart Failure
Abstract Body (Do not enter title and authors here): Introduction
Sepsis and systolic heart failure (sHF) often prompt hospitalization and require near diametrically opposite treatment strategies. We, therefore, studied whether sHF would impact outcomes in patients with sepsis spectra.
Methods
We examined the National Inpatient Sample 2021 for adults admitted with sepsis spectra (sepsis, severe sepsis, and septic shock). We compared patients with sHF vs those without. STATA 18th edition was used for analyses. Age, gender, race, hypertension, diabetes, obesity, dyslipidemia, and Elixhauser comorbidity index were identified as confounders by univariate analyses and tested further with multivariate logistic regression models. The primary outcome was mortality. Secondary outcomes were the need for intubation, cardiac arrest, length of stay (LOS), and total hospital charges.
Results
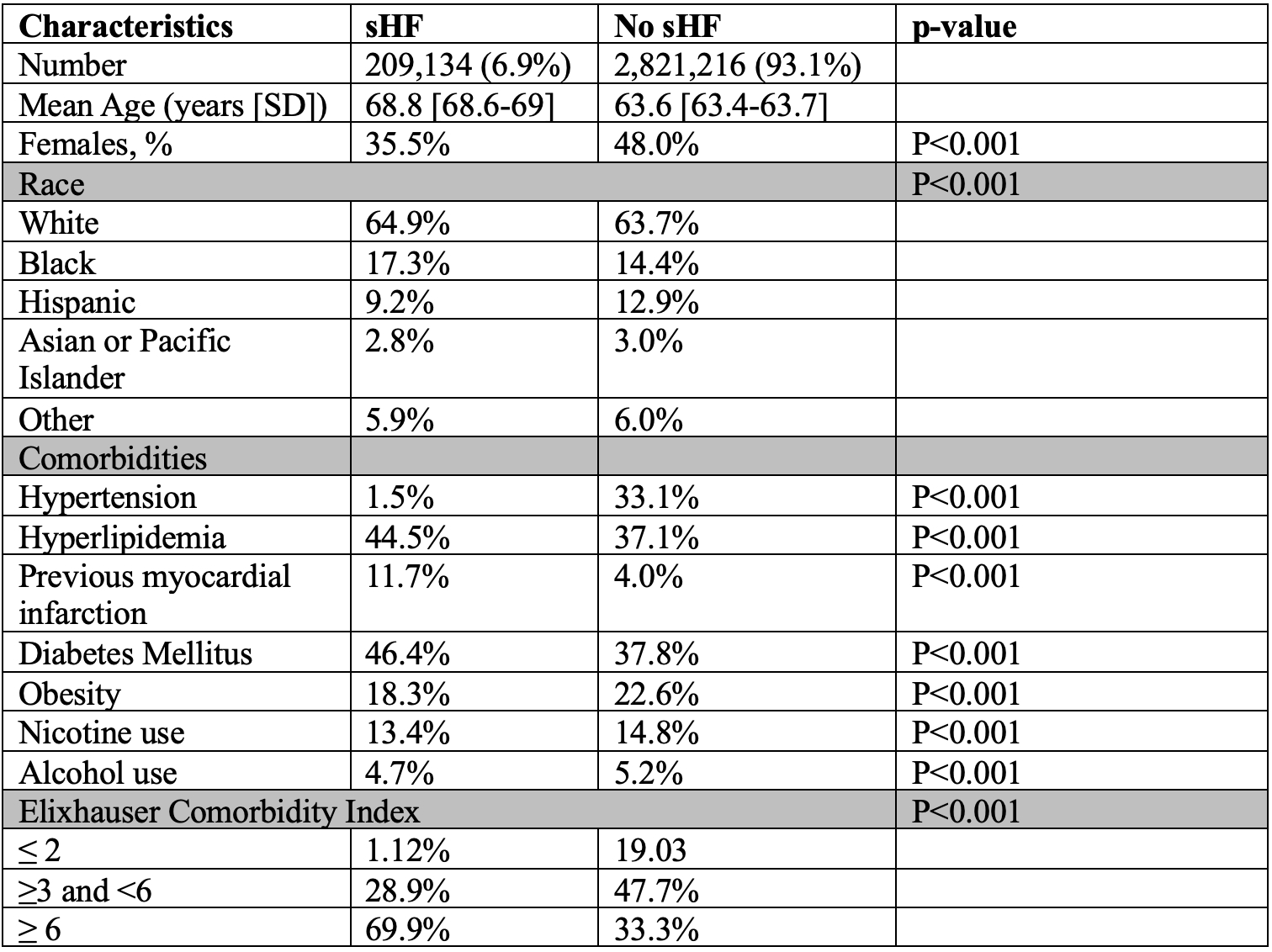
In 2021, nationwide, 3,030,351 adults were admitted for sepsis spectra, and 209,134 (6.9%) had concomitant sHF. Patients with sHF and sepsis spectra (as compared to those without sHF) were less likely female (35.5% vs. 48%), had a substantially higher likelihood of a prior MI, and nearly 50% were diabetic and hyperlipidemic with a higher comorbidity index. Baseline characteristics are in the Table.
Sepsis and sHF resulted in substantially higher mortality (22.7%) as compared to patients with sepsis alone (14.9%) adjusted odds ratio (aOR) of 1.11 (CI 1.08-1.14; p-value < 0.001). Patients with sepsis and sHF were more likely to require intubation 22.2% vs. 14.0% aOR 1.21 (CI 1.18-1.25; p-value < 0.001), had more cardiac arrest 7.7% vs. 4.0% aOR 1.38 (CI 1.32-1.44; p-value < 0.001), and a longer LOS (11.9 vs 9.4 days adjusted incidence rate ratio (aIRR) 1.06; CI 1.05 – 1.08; p-value < 0.001). Consequently, total hospital charges were also higher, $189,415 vs $133,720, aIRR 1.15 (CI 1.13-1.18; p-value < 0.001).
Conclusion
In 2021, nationwide, sepsis spectra remain a major cause of in-patient mortality. We demonstrate that the coexistence of systolic heart failure and sepsis dramatically worsens complications, mortality, and total hospital costs. This study is a call to action for the in-depth analyses of this very high-risk group of patients.
Sepsis and systolic heart failure (sHF) often prompt hospitalization and require near diametrically opposite treatment strategies. We, therefore, studied whether sHF would impact outcomes in patients with sepsis spectra.
Methods
We examined the National Inpatient Sample 2021 for adults admitted with sepsis spectra (sepsis, severe sepsis, and septic shock). We compared patients with sHF vs those without. STATA 18th edition was used for analyses. Age, gender, race, hypertension, diabetes, obesity, dyslipidemia, and Elixhauser comorbidity index were identified as confounders by univariate analyses and tested further with multivariate logistic regression models. The primary outcome was mortality. Secondary outcomes were the need for intubation, cardiac arrest, length of stay (LOS), and total hospital charges.
Results
In 2021, nationwide, 3,030,351 adults were admitted for sepsis spectra, and 209,134 (6.9%) had concomitant sHF. Patients with sHF and sepsis spectra (as compared to those without sHF) were less likely female (35.5% vs. 48%), had a substantially higher likelihood of a prior MI, and nearly 50% were diabetic and hyperlipidemic with a higher comorbidity index. Baseline characteristics are in the Table.
Sepsis and sHF resulted in substantially higher mortality (22.7%) as compared to patients with sepsis alone (14.9%) adjusted odds ratio (aOR) of 1.11 (CI 1.08-1.14; p-value < 0.001). Patients with sepsis and sHF were more likely to require intubation 22.2% vs. 14.0% aOR 1.21 (CI 1.18-1.25; p-value < 0.001), had more cardiac arrest 7.7% vs. 4.0% aOR 1.38 (CI 1.32-1.44; p-value < 0.001), and a longer LOS (11.9 vs 9.4 days adjusted incidence rate ratio (aIRR) 1.06; CI 1.05 – 1.08; p-value < 0.001). Consequently, total hospital charges were also higher, $189,415 vs $133,720, aIRR 1.15 (CI 1.13-1.18; p-value < 0.001).
Conclusion
In 2021, nationwide, sepsis spectra remain a major cause of in-patient mortality. We demonstrate that the coexistence of systolic heart failure and sepsis dramatically worsens complications, mortality, and total hospital costs. This study is a call to action for the in-depth analyses of this very high-risk group of patients.
More abstracts on this topic:
A Polypill Strategy for Heart Failure with Reduced Ejection Fraction: The POLY-HF Trial
Pandey Ambarish, Wang Thomas, Keshvani Neil, Rizvi Syed Kazim, Jain Anand, Coellar Juan David, Drazner Mark, Gupta Deepak, Chandra Alvin, Zaha Vlad
A Trial of Patients Receiving Remote Ischemic Conditioning in Early Stroke (PRICES) in a Tertiary Hospital in the Philippines: An Open Label StudyAng Kevin Royce, Juangco Dan, Hernandez Maria Kim