Final ID: Su2075
Outcomes of Left Atrial Appendage Occlusion With and Without Concurrent Catheter Ablation for Patients at High Bleeding Risk: A Systematic Review and Meta-analysis
Abstract Body (Do not enter title and authors here): Introduction:
The prevalence of non-valvular atrial fibrillation (NVAF) and stroke-related morbidity is rising. First-line therapy remains rate or rhythm control with anticoagulation, with catheter ablation (CA) also considered in suitable candidates. Left atrial appendage closure (LAAC) is increasingly used due to mounting evidence of non-inferiority compared to anticoagulation. Despite improved pre-procedural planning and patient selection reducing complications, adverse outcomes such as pericardial effusion and device-related thrombus occur in about 5% of patients. This study evaluates the outcomes of LAAC with CA versus standalone LAAC in NVAF patients with contraindications to anticoagulation.
Methods:
We searched PubMed, EMBASE, and Cochrane databases for all cohort studies comparing LAAC with CA to LAAC alone in patients with NVAF. Case series, reviews, and non-English language studies were excluded. The assessed outcomes included device compression rate at implant, device-related thrombosis, pericardial effusion, need for pericardiocentesis, and peri-device leak at 6 weeks. Statistical analysis was performed using Review Manager 5.1.7. Heterogeneity was assessed with I2 statistics.
Results:
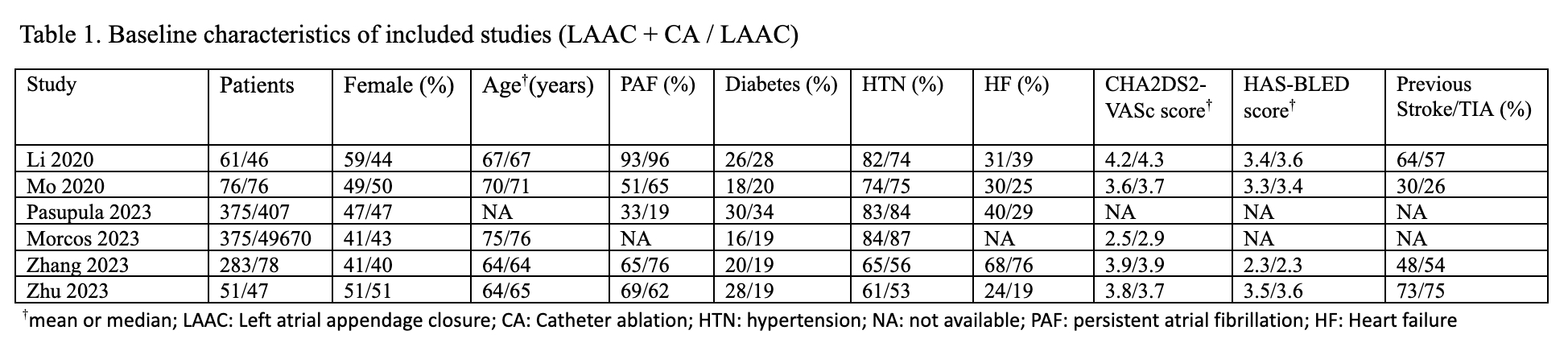
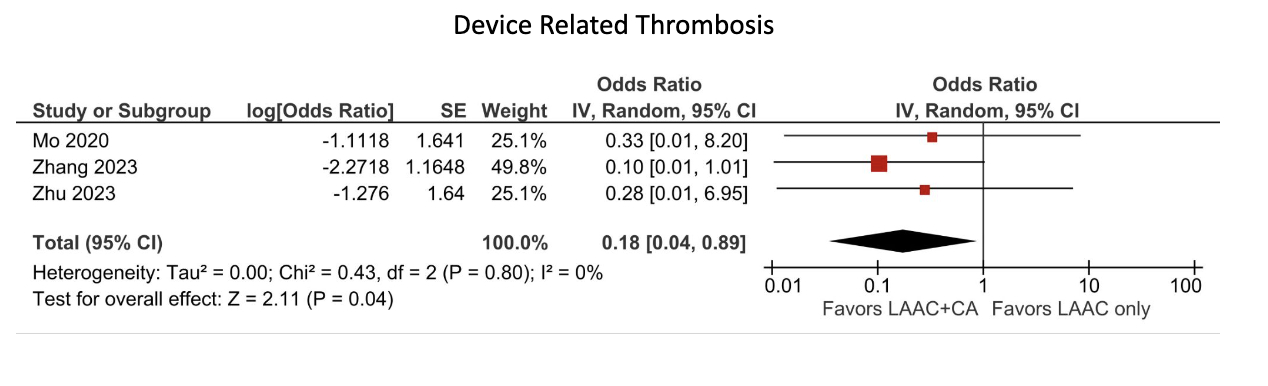
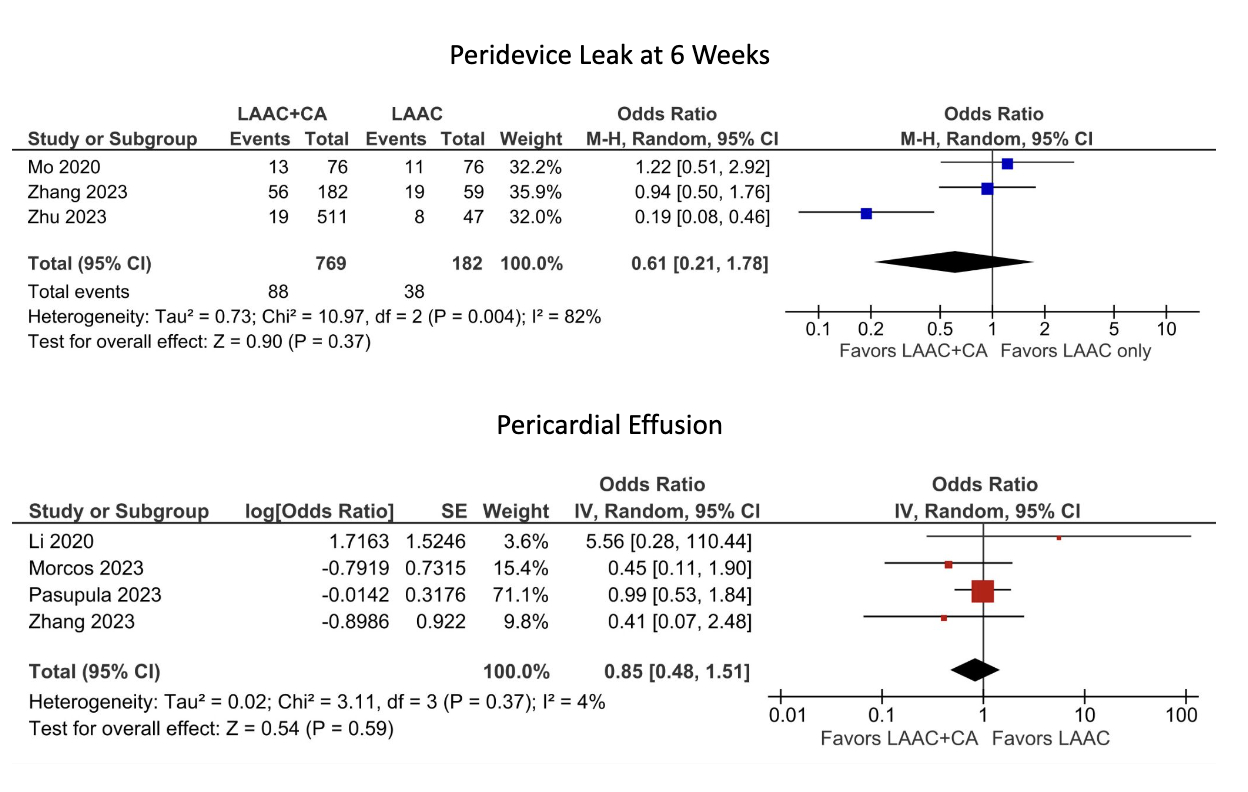
We included 6 studies with 51,545 patients, of whom 1,221 (2.3%) underwent both procedures. LAAC with CA and standalone LAAC cohorts had similar baseline demographics including age (68, 69 years), percentage of women (48%, 46%), CHA2DS2-VASc score (3.6, 3.7), and HAS-BLED score (3.1, 3.2). LAAC with CA was associated with a reduced incidence of device-related thrombosis (OR=0.18; 95% CI= 0.04-0.89; p=0.04) without an increase in pericardial effusion rates (OR=0.85; 95% CI= 0.48-1.51; p=0.59). There were no significant differences in device compression rates at implant (MD=0.34; 95% CI= -0.77-1.45; p=0.55), the need for pericardiocentesis (OR=1.01; 95% CI= 0.30-3.48; p=0.98), or rates of peri-device leak at 6 weeks (OR=0.61; 95% CI= 0.21-1.78; p=0.37).
Conclusion:
Concomitant LAAC with CA may reduce rates of device-related thrombosis compared to standalone LAAC without increasing the risk of pericardial effusion or peri-device leak at 6 weeks. These findings support the consideration of combining these procedures in the management of high-risk NVAF patients unable to tolerate anticoagulation.
The prevalence of non-valvular atrial fibrillation (NVAF) and stroke-related morbidity is rising. First-line therapy remains rate or rhythm control with anticoagulation, with catheter ablation (CA) also considered in suitable candidates. Left atrial appendage closure (LAAC) is increasingly used due to mounting evidence of non-inferiority compared to anticoagulation. Despite improved pre-procedural planning and patient selection reducing complications, adverse outcomes such as pericardial effusion and device-related thrombus occur in about 5% of patients. This study evaluates the outcomes of LAAC with CA versus standalone LAAC in NVAF patients with contraindications to anticoagulation.
Methods:
We searched PubMed, EMBASE, and Cochrane databases for all cohort studies comparing LAAC with CA to LAAC alone in patients with NVAF. Case series, reviews, and non-English language studies were excluded. The assessed outcomes included device compression rate at implant, device-related thrombosis, pericardial effusion, need for pericardiocentesis, and peri-device leak at 6 weeks. Statistical analysis was performed using Review Manager 5.1.7. Heterogeneity was assessed with I2 statistics.
Results:
We included 6 studies with 51,545 patients, of whom 1,221 (2.3%) underwent both procedures. LAAC with CA and standalone LAAC cohorts had similar baseline demographics including age (68, 69 years), percentage of women (48%, 46%), CHA2DS2-VASc score (3.6, 3.7), and HAS-BLED score (3.1, 3.2). LAAC with CA was associated with a reduced incidence of device-related thrombosis (OR=0.18; 95% CI= 0.04-0.89; p=0.04) without an increase in pericardial effusion rates (OR=0.85; 95% CI= 0.48-1.51; p=0.59). There were no significant differences in device compression rates at implant (MD=0.34; 95% CI= -0.77-1.45; p=0.55), the need for pericardiocentesis (OR=1.01; 95% CI= 0.30-3.48; p=0.98), or rates of peri-device leak at 6 weeks (OR=0.61; 95% CI= 0.21-1.78; p=0.37).
Conclusion:
Concomitant LAAC with CA may reduce rates of device-related thrombosis compared to standalone LAAC without increasing the risk of pericardial effusion or peri-device leak at 6 weeks. These findings support the consideration of combining these procedures in the management of high-risk NVAF patients unable to tolerate anticoagulation.
More abstracts on this topic:
A novel risk score predicts the prevalence of left atrial low-voltage areas and rhythm outcome in patients undergoing long-standing persistent atrial fibrillation ablation
Ooka Hirotaka, Nakao Sho, Kusuda Masaya, Ariyasu Wataru, Kudo Satoshi, Fujii Subaru, Mano Toshiaki, Matsuda Yasuhiro, Masuda Masaharu, Okamoto Shin, Ishihara Takayuki, Nanto Kiyonori, Tsujimura Takuya, Hata Yosuke, Uematsu Hiroyuki
Adherence to Guideline-Directed Oral Anticoagulant Therapy in Patients with Atrial Fibrillation and Atrial Flutter Admitted in a Tertiary Private Hospital: A Retrospective StudyWong Jasmine, Carandang Frances, Segundo Luigi Pierre