Final ID: Mo4026
Anticoagulation versus Antiplatelets in Coronary Artery Ectasia and Acute Coronary Syndrome: A Systematic Review and Meta-analysis
Abstract Body (Do not enter title and authors here): Introduction: Coronary artery ectasia (CAE) is a rare but well-recognized anatomical abnormality of the coronary arteries with a prevalence of up to 9% in patients presenting with acute coronary syndrome (ACS). While anticoagulants have been suggested to reduce recurrent events, the optimal antithrombotic therapy in CAE and ACS remains unclear.
Research Question: What is the comparative effect of anticoagulation therapy versus no anticoagulation in patients with CAE and ACS receiving background antiplatelet therapy?
Goals: To perform a systematic review and meta-analysis evaluating the efficacy of anticoagulation in preventing major adverse cardiovascular events (MACE) among patients with CAE and ACS.
Methods: We searched PubMed, Embase, and Cochrane to identify studies comparing the use of anticoagulants versus no use of anticoagulants as part of the antithrombotic therapy in patients presenting CAE and ACS, and reported MACE. Statistical analysis was performed using R version 4.2.2 adopting the Mantel-Haenszel random-effects model. Heterogeneity was assessed using Cochrane's Q statistic and Higgins and Thompson’s I2 statistics. Pooled risk ratios were used to evaluate the effectiveness of anticoagulant therapy in CAE and ACS.
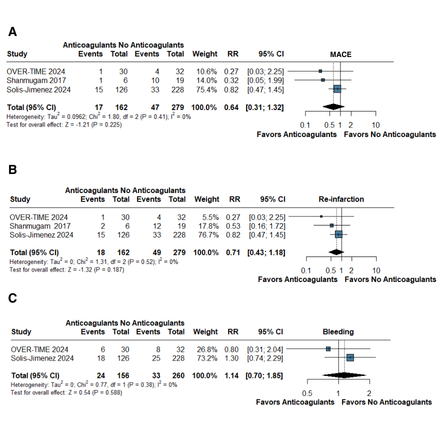
Results: We included 3 studies, including 1 randomized controlled trial and 2 observational studies, comprising a total of 441 patients, of whom 162 (36.7%) received anticoagulants, including vitamin K antagonists (warfarin and acenocoumarol) or direct oral anticoagulants (rivaroxaban, apixaban, and dabigatran). Time of follow-up ranged from 12 to 52 months, mean age was 57.9 ± 11.4 years, and 388 (87.9%) were male. We found no significant difference in MACE between patients who received anticoagulation and patients who did not (RR 0.64; 95% CI 0.31, 1.32; p=0.22; I2 = 0%). Additionally, there was no difference in the risk of re-infarction (RR 0.71; 95% CI 0.43, 1.18; p=0.19; I2 = 0%). Finally, there was no significant difference in risk of bleeding between both groups (RR 1.41; 95% CI 0.70, 1.85; p=0.19; I2 = 0.59%).
Conclusion: Our findings suggest that, among patients with CAE and ACS, anticoagulation does not reduce the risk of MACE or re-infarction as compared with no anticoagulation.
Research Question: What is the comparative effect of anticoagulation therapy versus no anticoagulation in patients with CAE and ACS receiving background antiplatelet therapy?
Goals: To perform a systematic review and meta-analysis evaluating the efficacy of anticoagulation in preventing major adverse cardiovascular events (MACE) among patients with CAE and ACS.
Methods: We searched PubMed, Embase, and Cochrane to identify studies comparing the use of anticoagulants versus no use of anticoagulants as part of the antithrombotic therapy in patients presenting CAE and ACS, and reported MACE. Statistical analysis was performed using R version 4.2.2 adopting the Mantel-Haenszel random-effects model. Heterogeneity was assessed using Cochrane's Q statistic and Higgins and Thompson’s I2 statistics. Pooled risk ratios were used to evaluate the effectiveness of anticoagulant therapy in CAE and ACS.
Results: We included 3 studies, including 1 randomized controlled trial and 2 observational studies, comprising a total of 441 patients, of whom 162 (36.7%) received anticoagulants, including vitamin K antagonists (warfarin and acenocoumarol) or direct oral anticoagulants (rivaroxaban, apixaban, and dabigatran). Time of follow-up ranged from 12 to 52 months, mean age was 57.9 ± 11.4 years, and 388 (87.9%) were male. We found no significant difference in MACE between patients who received anticoagulation and patients who did not (RR 0.64; 95% CI 0.31, 1.32; p=0.22; I2 = 0%). Additionally, there was no difference in the risk of re-infarction (RR 0.71; 95% CI 0.43, 1.18; p=0.19; I2 = 0%). Finally, there was no significant difference in risk of bleeding between both groups (RR 1.41; 95% CI 0.70, 1.85; p=0.19; I2 = 0.59%).
Conclusion: Our findings suggest that, among patients with CAE and ACS, anticoagulation does not reduce the risk of MACE or re-infarction as compared with no anticoagulation.
More abstracts on this topic:
Anticoagulant therapy for cerebral venous sinus thrombosis: A propensity score matching study
Liu Kai, Wei Zhao, Meng Zhang, Qin Dai, Song Bo, Xu Yuming
Antithrombotic Therapy for Secondary Stroke Prevention in Patients with Severe Chronic Kidney Disease and Atrial FibrillationJones Erica, Peterson Eric, Xian Ying, Ayodele Iyanuoluwa, Obrien Emily, Laskowitz Daniel, Fonarow Gregg, Matsouaka Roland, Schwamm Lee, Smith Eric, Bhatt Deepak