Final ID: MDP639
The Effect of Periprocedural Statin Therapy on Mortality and Cardiovascular Outcomes in Patients Undergoing Transcatheter Aortic Valve Replacement: A Systematic Review and Meta-Analysis
Abstract Body (Do not enter title and authors here):
Background
Transcatheter aortic valve replacement (TAVR) stands as a notable alternative to surgery for severe aortic stenosis (AS). Despite the established benefits of statins in cardiovascular pathologies, their specific impact in patients with severe AS undergoing TAVR remains uncertain. Our study aims to assess whether perioperative statin use improves survival and outcomes post-TAVR.
Methods
A search was conducted across various databases to retrieve studies comparing perioperative statin use versus no statin use in patients undergoing TAVR. The primary outcome of interest was all-cause mortality (ACM). Secondary outcomes included stroke, acute kidney injury (AKI), 30-day mortality, myocardial infarction (MI), cardiovascular complications, and in-hospital mortality. Comprehensive Meta-Analysis Software (v. 3) was used to pool odds ratio (OR) under a random-effects model, with statistical significance set at p < 0.05.
Results
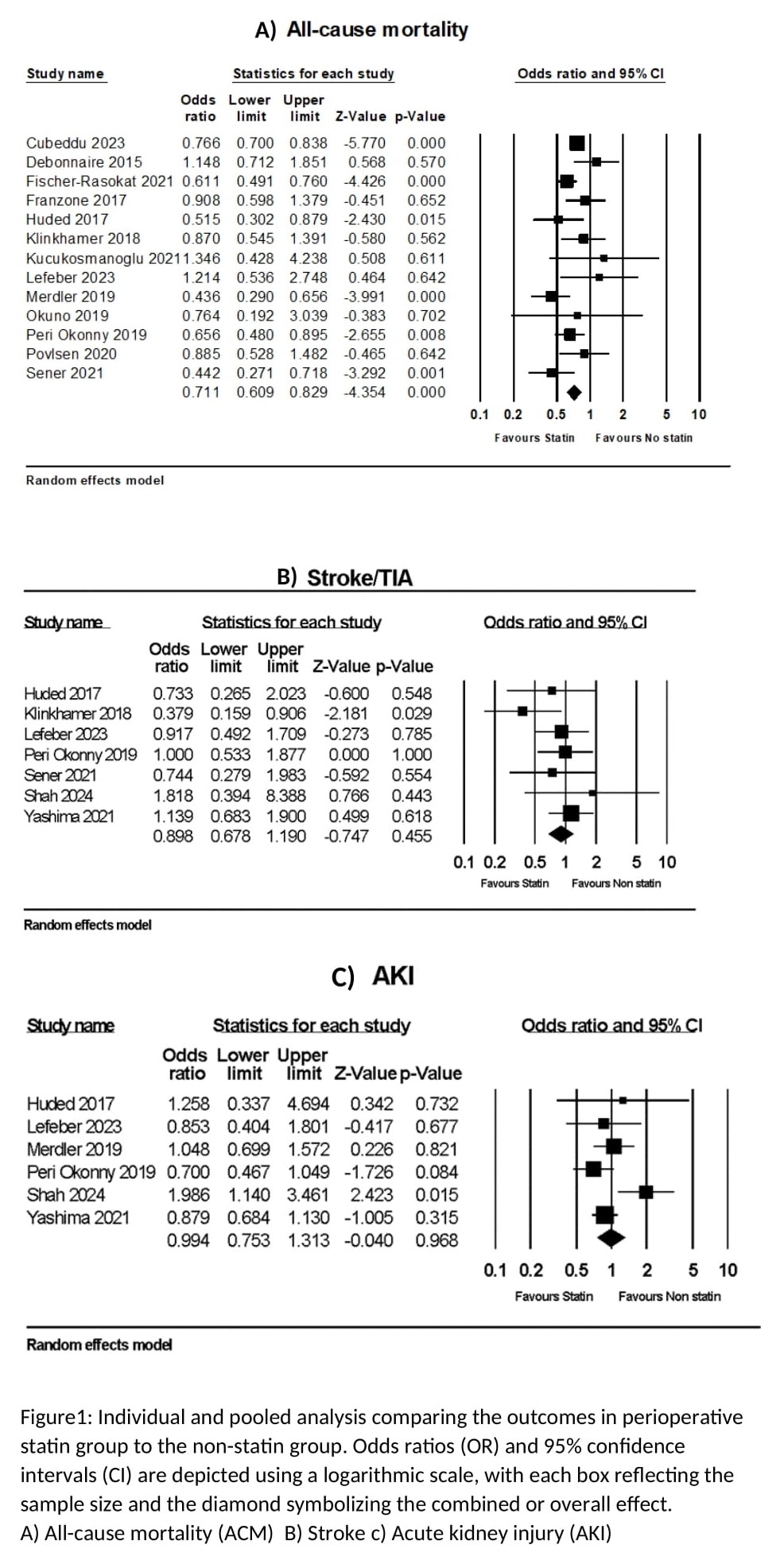
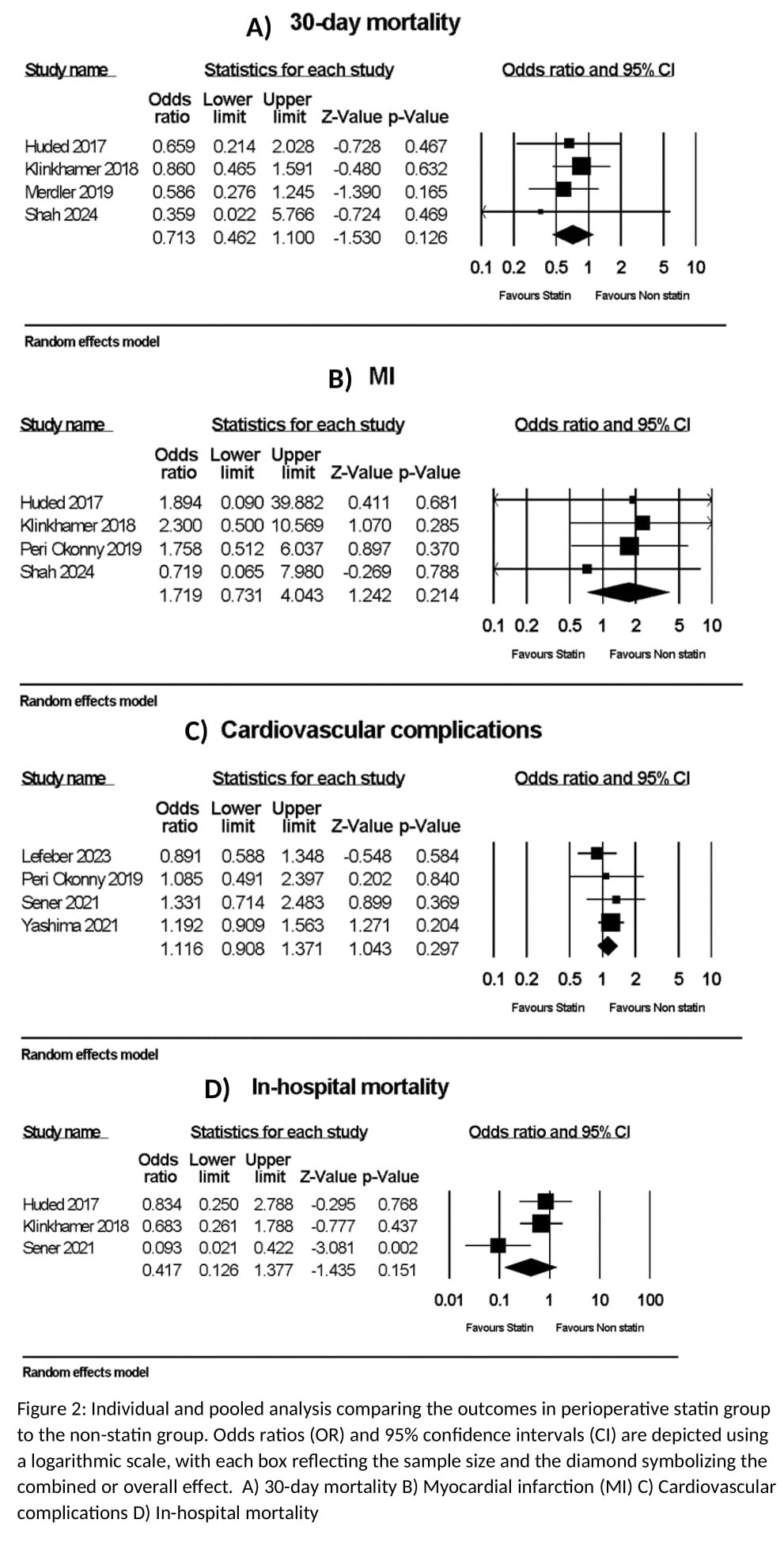
Our analysis encompassing 20663 patients from 15 observational studies found that perioperative statin use was associated with a significant reduction in ACM (OR= 0.71, 95% CI: 0.61-0.83, I2= 50.3%, p<0.001). Although not statistically significant, perioperative statin use demonstrated a trend towards a decreased risk of stroke (OR= 0.90, 95% CI: 0.68-1.19, I2= 0%, p= 0.455), AKI (OR= 0.99, 95% CI: 0.75-1.31, I2= 49%, p= 0.968), and 30-day mortality (OR= 0.71, 95% CI: 0.46-1.10, I2= 0%, p= 0.126), and no difference was seen in the risk of MI (OR= 1.72, 95% CI: 0.73-4.04, I2= 0%, p= 0.214), cardiovascular complications (OR= 1.12, 95% CI: 0.91-1.37, I2= 0%, p= 0.297), and in-hospital mortality (OR= 0.42, 95% CI: 0.13-1.38, I2= 65.8%, p= 0.151) (Figure 1 and 2).
Conclusion
Perioperative statin therapy reduces all-cause mortality in TAVR patients but shows limited impact on other outcomes. Further large-scale prospective studies and trials are necessary to corroborate our findings.
Background
Transcatheter aortic valve replacement (TAVR) stands as a notable alternative to surgery for severe aortic stenosis (AS). Despite the established benefits of statins in cardiovascular pathologies, their specific impact in patients with severe AS undergoing TAVR remains uncertain. Our study aims to assess whether perioperative statin use improves survival and outcomes post-TAVR.
Methods
A search was conducted across various databases to retrieve studies comparing perioperative statin use versus no statin use in patients undergoing TAVR. The primary outcome of interest was all-cause mortality (ACM). Secondary outcomes included stroke, acute kidney injury (AKI), 30-day mortality, myocardial infarction (MI), cardiovascular complications, and in-hospital mortality. Comprehensive Meta-Analysis Software (v. 3) was used to pool odds ratio (OR) under a random-effects model, with statistical significance set at p < 0.05.
Results
Our analysis encompassing 20663 patients from 15 observational studies found that perioperative statin use was associated with a significant reduction in ACM (OR= 0.71, 95% CI: 0.61-0.83, I2= 50.3%, p<0.001). Although not statistically significant, perioperative statin use demonstrated a trend towards a decreased risk of stroke (OR= 0.90, 95% CI: 0.68-1.19, I2= 0%, p= 0.455), AKI (OR= 0.99, 95% CI: 0.75-1.31, I2= 49%, p= 0.968), and 30-day mortality (OR= 0.71, 95% CI: 0.46-1.10, I2= 0%, p= 0.126), and no difference was seen in the risk of MI (OR= 1.72, 95% CI: 0.73-4.04, I2= 0%, p= 0.214), cardiovascular complications (OR= 1.12, 95% CI: 0.91-1.37, I2= 0%, p= 0.297), and in-hospital mortality (OR= 0.42, 95% CI: 0.13-1.38, I2= 65.8%, p= 0.151) (Figure 1 and 2).
Conclusion
Perioperative statin therapy reduces all-cause mortality in TAVR patients but shows limited impact on other outcomes. Further large-scale prospective studies and trials are necessary to corroborate our findings.
More abstracts on this topic:
A Body Shape Index at Age 25-64 Predicts Mortality and CHD Hospitalization
Shafran Itamar, Krakauer Nir, Krakauer Jesse, Cohen Gali, Gerber Yariv
Activin Signaling Inhibition Enhances Cardiac Functional Recovery After Aortic DebandingSingh Anand, Guseh James Sawalla, Xiao Chunyang, Babbs Keith, Seehra Jasbir, Li Haobo, Rosenzweig Anthony