Final ID: Su302
Impact of Time to Defibrillation on Mortality after In-Hospital Cardiac Arrest
Abstract Body: Background
In-hospital cardiac arrest occurs in 290,000 patients annually in the United States, with less than 20% of these arrests featuring a shockable presenting rhythm. The three-phase model of CPR is separated into the electrical phase which occurs in the first 4 minutes, the circulatory phase which includes minutes 4-10, and the metabolic phase which is greater than 10 minutes from arrest onset. Defibrillation during the electrical phase has been proven to improve survival by approximately 50%. Current guidelines recommend defibrillation within the first 2 minutes of arrest in those with a rhythm of VT/VF.
The purpose of this study was to determine the effect of time to defibrillation on mortality in patients with shockable rhythms.
Methods
Full-disclosure rhythm strips for all cardiac arrests in non-ICU patients on telemetry were reviewed from Feb 2019 to April 2023. Time to defibrillation of shockable rhythms (VT/VF) was determined from the telemetry data and corresponding defibrillator data from the Zoll CodeNet electronic system.
Results
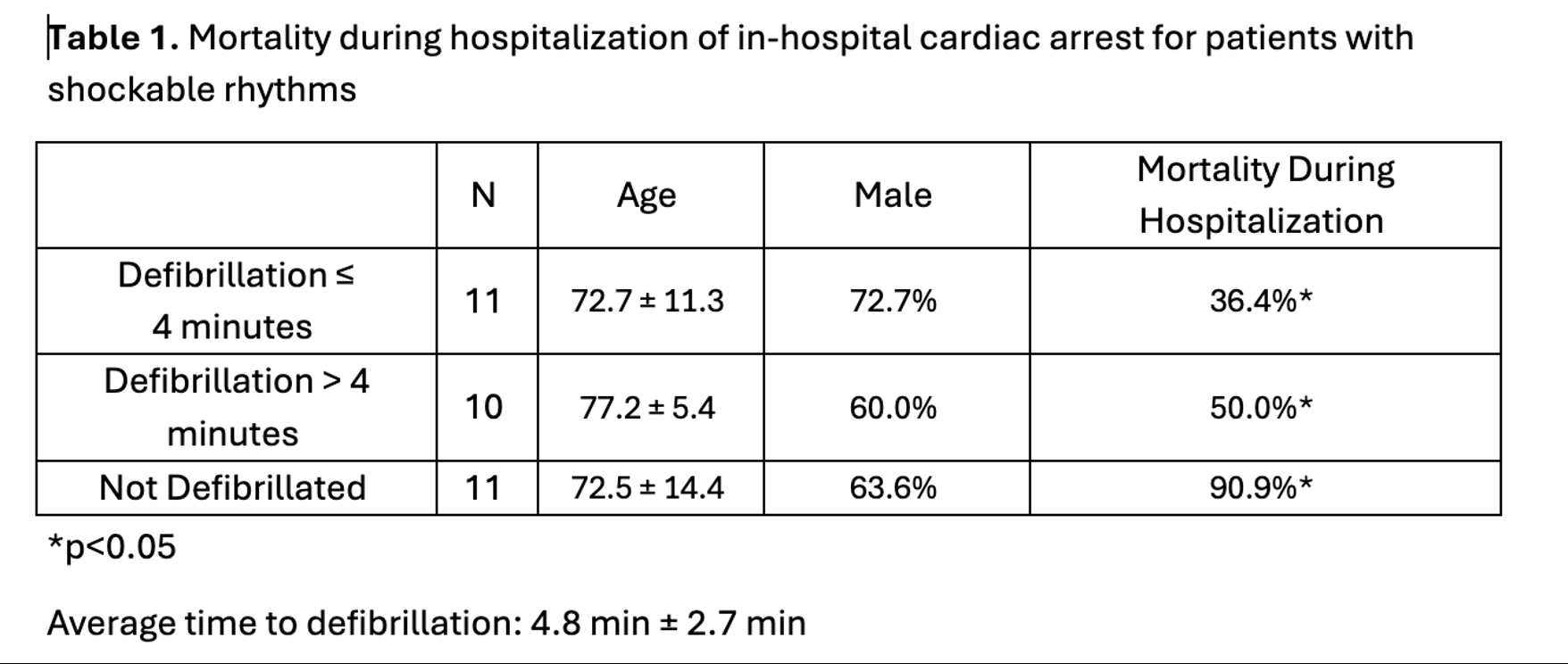
We identified 32 of the 186 patients with cardiac arrest while on telemetry presenting with pulseless monomorphic VTor polymorphic VT/VF. The average time to defibrillation was 4.8 min ± 2.7 min. 34% of patients were defibrillated in 4 minutes or less from the onset of the arrythmia, 31% were defibrillated in more than 4 minutes from the onset of the arrythmia, and 34% were not defibrillated. Patients defibrillated in 4 minutes or less had a significantly lower mortality of 36.4% compared to a 50% mortality of those defibrillated in more than 4 minutes and 90.9% mortality in those not defibrillated (p<0.05).The patients who were not defibrillated were determined to have ongoing VT or poly VT/VF until telemetry was removed and the Zoll defibrillator pads were applied. They were ultimately deermined ot have PEA and were not shocked.
Conclusions
Patients defibrillated in 4 minutes or less from the onset of a sustained shockable arrythmia experienced significantly lower mortality during hospitalization compared to those who were defibrillated in more than 4 minutes or were not defibrillated. 34% of patients with a shockable rhythm were not defibrillated due to a diagnosis of PEA after the Zoll pads were placed. Patients with sustained VT/VF causing in-hospital cardiac arrest should be defibrillated as soon as a defibrillator can be applied. Telemetry data should be clearly communicated to the code team.
In-hospital cardiac arrest occurs in 290,000 patients annually in the United States, with less than 20% of these arrests featuring a shockable presenting rhythm. The three-phase model of CPR is separated into the electrical phase which occurs in the first 4 minutes, the circulatory phase which includes minutes 4-10, and the metabolic phase which is greater than 10 minutes from arrest onset. Defibrillation during the electrical phase has been proven to improve survival by approximately 50%. Current guidelines recommend defibrillation within the first 2 minutes of arrest in those with a rhythm of VT/VF.
The purpose of this study was to determine the effect of time to defibrillation on mortality in patients with shockable rhythms.
Methods
Full-disclosure rhythm strips for all cardiac arrests in non-ICU patients on telemetry were reviewed from Feb 2019 to April 2023. Time to defibrillation of shockable rhythms (VT/VF) was determined from the telemetry data and corresponding defibrillator data from the Zoll CodeNet electronic system.
Results
We identified 32 of the 186 patients with cardiac arrest while on telemetry presenting with pulseless monomorphic VTor polymorphic VT/VF. The average time to defibrillation was 4.8 min ± 2.7 min. 34% of patients were defibrillated in 4 minutes or less from the onset of the arrythmia, 31% were defibrillated in more than 4 minutes from the onset of the arrythmia, and 34% were not defibrillated. Patients defibrillated in 4 minutes or less had a significantly lower mortality of 36.4% compared to a 50% mortality of those defibrillated in more than 4 minutes and 90.9% mortality in those not defibrillated (p<0.05).The patients who were not defibrillated were determined to have ongoing VT or poly VT/VF until telemetry was removed and the Zoll defibrillator pads were applied. They were ultimately deermined ot have PEA and were not shocked.
Conclusions
Patients defibrillated in 4 minutes or less from the onset of a sustained shockable arrythmia experienced significantly lower mortality during hospitalization compared to those who were defibrillated in more than 4 minutes or were not defibrillated. 34% of patients with a shockable rhythm were not defibrillated due to a diagnosis of PEA after the Zoll pads were placed. Patients with sustained VT/VF causing in-hospital cardiac arrest should be defibrillated as soon as a defibrillator can be applied. Telemetry data should be clearly communicated to the code team.
More abstracts on this topic:
Association of Epicardial Adipose Tissue with Lipomatous Metaplasia and Ventricular Tachycardia Recurrence Following Ablation in Patients with Non-Ischemic Cardiomyopathy
Xu Lingyu, Liao Ting-wei Ernie, Callans David, Marchlinski Francis, Witschey Walter, Desjardins Benoit, Nazarian Saman
All Things in Moderation: Right Ventricular Moderator Band Induced Ventricular Fibrillation In A Young MaleKamran Wali, Pusukur Bharani, Sutton Peter, Rao Yash, Deboer Rebecca, Al-mohamad Talal, Cossu Sergio, Patel Kunal