Final ID: Su1205
The Effect of Targeted Temperature Management on Five-Year Mortality in Comatose Out-of-Hospital Cardiac Arrest Survivors: A Real-World Experience
Abstract Body: Background:
Hypothermia-Induced Targeted Temperature Management (TTM) is a neuroprotective treatment after the return of spontaneous circulation (ROSC) in comatose survivors of out-of-hospital cardiac arrest (OHCA). However, its effectiveness in all patient subpopulations is debated. While short-term survival has been well studied, the impact of TTM on long-term survival is still unknown.
Methods:
In a prospective cohort study, 98 comatose survivors of non-traumatic OHCA were recruited from four tertiary-level hospitals in Buffalo, Western New York and followed up for five years. Patients with active cancer, infection, cardiac pathology or surgery in three-month prior to presentation, were excluded. Cardiac arrest characteristics, demographics, comorbidities, and therapeutic interventions were recorded. According to TTM protocols, a target body temperature of 33°C was reached and maintained for 24 hours using either an intravascular cooling catheter or a surface cooling system. This was followed by gradual controlled rewarming over 12-24 hours to normothermia. Factors associated with the receipt of TTM were determined. The effect of TTM on five-year survival was studied using cox-regression analysis.
Results:
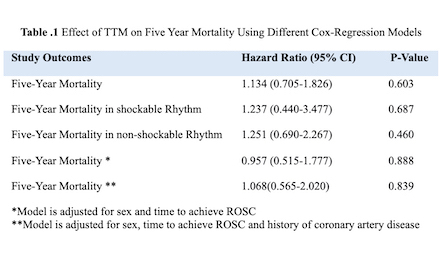
Among comatose patients with mean age of 60.1±14.9 years, 49% received TTM. Females were significantly less likely to receive TTM (35.1% vs 59.3%, p=0.021). In TTM group, the time to ROSC was significantly longer: median [IQR] 14.5 mins (5-19.7) vs 20 mins (12-27), p=0.018. TTM group was more likely to have a history of coronary artery disease (CAD) (12.5% vs 35.4%, p=0.009). Overall, 5-year mortality did not differ significantly between TTM vs. non-TTM: 72.9% vs 66.0%, (HR: 1.134, 95% CI: 0.705-1.826, p=0.603) in univariate and multivariate Cox-regression analysis (Table 1).
Conclusion:
While females are less likely to receive TTM treatment, TTM is more likely to be used in patients with a longer time to ROSC and a history of CAD. The overall five-year survival remains high in both treatment groups in all eligible patients, as well as in shockable and non-shockable rhythm groups studied separately. Larger cohort studies are needed to determine the patients who may benefit most from TTM.
Hypothermia-Induced Targeted Temperature Management (TTM) is a neuroprotective treatment after the return of spontaneous circulation (ROSC) in comatose survivors of out-of-hospital cardiac arrest (OHCA). However, its effectiveness in all patient subpopulations is debated. While short-term survival has been well studied, the impact of TTM on long-term survival is still unknown.
Methods:
In a prospective cohort study, 98 comatose survivors of non-traumatic OHCA were recruited from four tertiary-level hospitals in Buffalo, Western New York and followed up for five years. Patients with active cancer, infection, cardiac pathology or surgery in three-month prior to presentation, were excluded. Cardiac arrest characteristics, demographics, comorbidities, and therapeutic interventions were recorded. According to TTM protocols, a target body temperature of 33°C was reached and maintained for 24 hours using either an intravascular cooling catheter or a surface cooling system. This was followed by gradual controlled rewarming over 12-24 hours to normothermia. Factors associated with the receipt of TTM were determined. The effect of TTM on five-year survival was studied using cox-regression analysis.
Results:
Among comatose patients with mean age of 60.1±14.9 years, 49% received TTM. Females were significantly less likely to receive TTM (35.1% vs 59.3%, p=0.021). In TTM group, the time to ROSC was significantly longer: median [IQR] 14.5 mins (5-19.7) vs 20 mins (12-27), p=0.018. TTM group was more likely to have a history of coronary artery disease (CAD) (12.5% vs 35.4%, p=0.009). Overall, 5-year mortality did not differ significantly between TTM vs. non-TTM: 72.9% vs 66.0%, (HR: 1.134, 95% CI: 0.705-1.826, p=0.603) in univariate and multivariate Cox-regression analysis (Table 1).
Conclusion:
While females are less likely to receive TTM treatment, TTM is more likely to be used in patients with a longer time to ROSC and a history of CAD. The overall five-year survival remains high in both treatment groups in all eligible patients, as well as in shockable and non-shockable rhythm groups studied separately. Larger cohort studies are needed to determine the patients who may benefit most from TTM.
More abstracts on this topic:
ADAR1 inhibiting ZBP1-driven neuronal necroptosis to improve secondary injury after intracerebral hemorrhage
Wang Shuoyang, Zhao Shoucai, Wu Xiaodong, Chu Zhaohu, Xu Yang
Beyond Repair: Resurrecting Neurons through Stem Cell TherapyHamdan Tesnim, Witt Iryna, Ascandar Nameer, Basaran Ali, Brewer Yukiko A., Chyshkevych Iryna