Final ID: LBP10
Impact of Door-In-Door-Out Times on Functional Outcomes in Patients with Stroke Transferred for Endovascular Therapy
Abstract Body: Intro: Interhospital transfer (IHT) is often required for endovascular therapy (EVT) for acute ischemic stroke (AIS) patients. The door-in-door-out (DIDO) times for patients who require EVT are often longer than the recommended 90 min (excellent) or 120 min (adequate) targets; yet, it is unknown how delays impact functional outcomes.
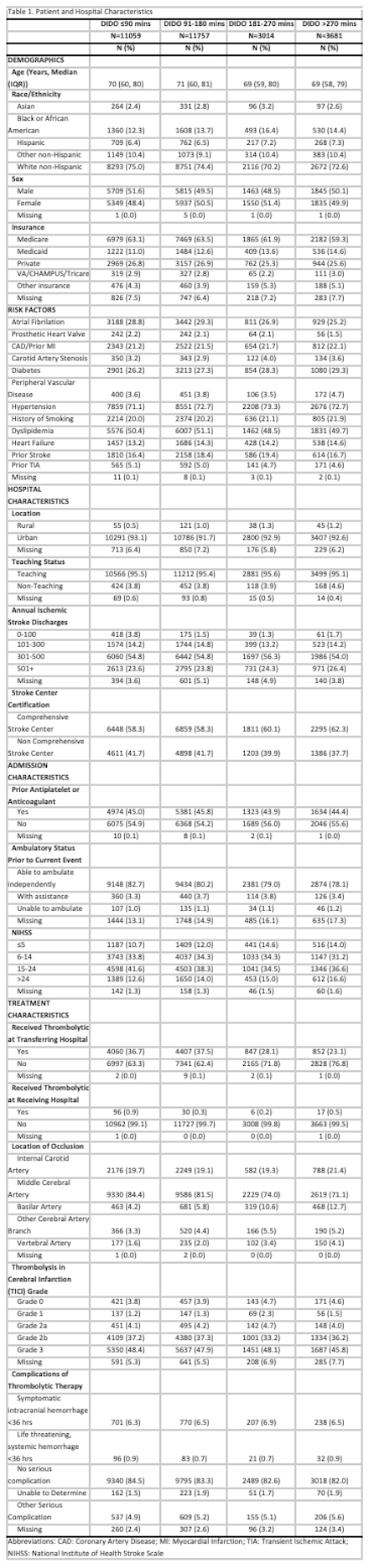
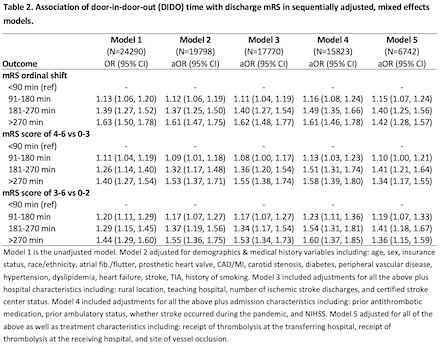
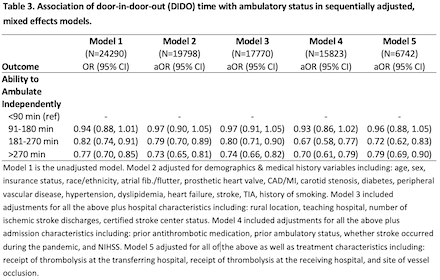
Methods: This was a cohort study of prospectively collected data of patients in the American Heart Association Get With The Guidelines®-Stroke registry with AIS who underwent EVT from Jan 2019 to Dec 2023 and were transferred from the ED at the presenting hospital to a thrombectomy-performing hospital. Patients were included if a potential target lesion for EVT was visualized during CT, MR, or catheter angiography. The primary outcome was level of disability at discharge (ordinal modified Rankin Scale, mRS); secondary outcomes included discharge ambulatory status (without assistance/with assistance/non-ambulatory/death) and mRS dichotomies at discharge of ambulatory and of self-care capable (mRS 0-3) and functional independence (mRS 0-2). Mixed effects models with random intercepts to account for clustering by hospital were used with sequential adjustment for demographics and risk factors, hospital characteristics, patient characteristics on admission to the thrombectomy hospital (including NIHSS score), and treatment characteristics (including use of intravenous thrombolysis, TICI reperfusion status, LVO location, and post-procedure complications).
Results: Among 29,511 patients (50.3% male, mean age 68.8 [SD:14.6] years, 74.0% White), 37.5% had DIDO time ≤90 mins, 39.8% 91-180 mins, 10.2% 181-270 mins, and 12.5% were >270 mins. In the model fully adjusting for arrival characteristics (Model 4), patients with longer DIDO times had higher odds of a one-point increase in discharge mRS (91-180 vs ≤90 mins: aOR 1.16 (95% CI 1.08, 1.24); 181-270 vs ≤90 mins: aOR 1.49 (95% CI 1.35, 1.66); >270 vs ≤90 mins: aOR 1.61 (95% CI 1.46, 1.78). This relationship remained when controlling for treatment characteristics (Model 5). Similar statistically significant increases in unfavorable outcomes with longer DIDO were observed for all secondary outcomes.
Discussion: Longer DIDO times were associated with greater disability outcomes and reduced independent ambulation at discharge in AIS patients transferred for EVT. Further efforts must be made to optimize the rapid evaluation and interhospital transfer of stroke patients eligible for EVT.
Methods: This was a cohort study of prospectively collected data of patients in the American Heart Association Get With The Guidelines®-Stroke registry with AIS who underwent EVT from Jan 2019 to Dec 2023 and were transferred from the ED at the presenting hospital to a thrombectomy-performing hospital. Patients were included if a potential target lesion for EVT was visualized during CT, MR, or catheter angiography. The primary outcome was level of disability at discharge (ordinal modified Rankin Scale, mRS); secondary outcomes included discharge ambulatory status (without assistance/with assistance/non-ambulatory/death) and mRS dichotomies at discharge of ambulatory and of self-care capable (mRS 0-3) and functional independence (mRS 0-2). Mixed effects models with random intercepts to account for clustering by hospital were used with sequential adjustment for demographics and risk factors, hospital characteristics, patient characteristics on admission to the thrombectomy hospital (including NIHSS score), and treatment characteristics (including use of intravenous thrombolysis, TICI reperfusion status, LVO location, and post-procedure complications).
Results: Among 29,511 patients (50.3% male, mean age 68.8 [SD:14.6] years, 74.0% White), 37.5% had DIDO time ≤90 mins, 39.8% 91-180 mins, 10.2% 181-270 mins, and 12.5% were >270 mins. In the model fully adjusting for arrival characteristics (Model 4), patients with longer DIDO times had higher odds of a one-point increase in discharge mRS (91-180 vs ≤90 mins: aOR 1.16 (95% CI 1.08, 1.24); 181-270 vs ≤90 mins: aOR 1.49 (95% CI 1.35, 1.66); >270 vs ≤90 mins: aOR 1.61 (95% CI 1.46, 1.78). This relationship remained when controlling for treatment characteristics (Model 5). Similar statistically significant increases in unfavorable outcomes with longer DIDO were observed for all secondary outcomes.
Discussion: Longer DIDO times were associated with greater disability outcomes and reduced independent ambulation at discharge in AIS patients transferred for EVT. Further efforts must be made to optimize the rapid evaluation and interhospital transfer of stroke patients eligible for EVT.
More abstracts on this topic:
Chest Compressions to the Left of the Sternum are Associated with Higher Systolic Blood Pressure than to the Lower Sternum
Frank Kevin, Cohen Allison, Haddad Ghania, Berruti Alaina, Li Timmy, Young Elizabeth, Becker Lance, Jafari Daniel, Rolston Daniel
A Randomized, Double Blinded, Phase 2B Clinical Trial to Compare the Safety and Efficacy of Sodium Chloride and Sodium Acetate Combination Intravenous Fluids in Acute Stroke PatientsWasay Muhammad, Suri Fareed, Saleem Shafaq, Qureshi Adnan
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)