Final ID: LB18
Coordinated, Collaborative, Comprehensive, Family-based, Integrated, Technology-enabled Post-Stroke Care
Abstract Body: Objective. To determine the effectiveness, defined at 12-months post-stroke discharge, of post-stroke care delivered using the Joint Commission (JC)-certified Comprehensive or Primary Care (CSC/PSC) model compared to an integrated, coordinated, technology-enabled Integrated Stroke Practice Unit (ISPU) model (that includes CSC/PSC care).
Background. Following stroke, patients face persisting physical/cognitive impairments, including loss of independence, functional/cognitive deficits, depression, and recurrence risk. Caregivers experience increased strain and limited support for complex disease management. US stroke care utilizes JC hospital certifications based on level of care provision with proven care processes in acute and in-hospital care, but post-discharge care for risk factor management and secondary prevention is limited. An ISPU integrates technology with proactive, team-based stroke care coordinated across the continuum for multiple specialties and has been shown effective for risk factor control and patient satisfaction in a single-site non-randomized demonstration study.
Design/Methods. C3FIT (Coordinated, Collaborative, Comprehensive, Family-based, Integrated, Technology-enabled Stroke Care) is a pragmatic cluster-randomized trial. US clinical sites (n=23) were stratified by patient volume and geography and randomized at the site level to continue CSC/PSC care or shift to CSC/PSC plus ISPU care. Eligibility was broad, including ischemic and hemorrhagic stroke, with ~100/site sample size. After hospital discharge, enrolled participants/caregivers were followed monthly for 12 visits (ISPU) or for three visits (CSC/PSC). Primary outcomes were functional (Modified Rankin Score) and health-related quality of life (Stroke Impact Scale) at 12-months post-discharge.
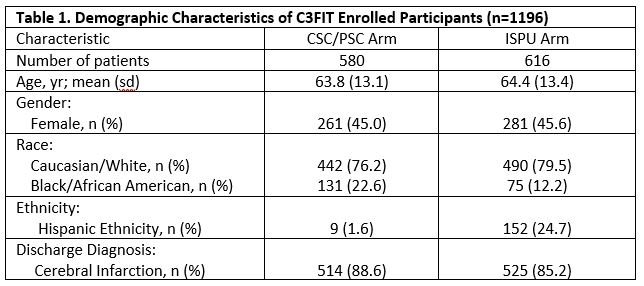
Results. The primary outcome analysis for the C3FIT trial will be presented (investigators currently masked pending follow-up completion). Enrollment began in March 2020 and ended in September 2023, and follow-up ended in October 2024.Total enrolled was 1,196 (580 CSC/PSC and 616 ISPU) at 21 clinical sites; of those, 196 patients were lost to follow-up (52 CSC/PSC and 144 ISPU). Table 1 describes demographic characteristics of C3FIT’s enrolled participants.
Conclusion. Primary results for the C3FIT trial will be presented. Post-stroke, patients face continued risk for decreased cognitive/physical disability and quality of life. C3FIT’s results may contribute to improved post-stroke care.
Background. Following stroke, patients face persisting physical/cognitive impairments, including loss of independence, functional/cognitive deficits, depression, and recurrence risk. Caregivers experience increased strain and limited support for complex disease management. US stroke care utilizes JC hospital certifications based on level of care provision with proven care processes in acute and in-hospital care, but post-discharge care for risk factor management and secondary prevention is limited. An ISPU integrates technology with proactive, team-based stroke care coordinated across the continuum for multiple specialties and has been shown effective for risk factor control and patient satisfaction in a single-site non-randomized demonstration study.
Design/Methods. C3FIT (Coordinated, Collaborative, Comprehensive, Family-based, Integrated, Technology-enabled Stroke Care) is a pragmatic cluster-randomized trial. US clinical sites (n=23) were stratified by patient volume and geography and randomized at the site level to continue CSC/PSC care or shift to CSC/PSC plus ISPU care. Eligibility was broad, including ischemic and hemorrhagic stroke, with ~100/site sample size. After hospital discharge, enrolled participants/caregivers were followed monthly for 12 visits (ISPU) or for three visits (CSC/PSC). Primary outcomes were functional (Modified Rankin Score) and health-related quality of life (Stroke Impact Scale) at 12-months post-discharge.
Results. The primary outcome analysis for the C3FIT trial will be presented (investigators currently masked pending follow-up completion). Enrollment began in March 2020 and ended in September 2023, and follow-up ended in October 2024.Total enrolled was 1,196 (580 CSC/PSC and 616 ISPU) at 21 clinical sites; of those, 196 patients were lost to follow-up (52 CSC/PSC and 144 ISPU). Table 1 describes demographic characteristics of C3FIT’s enrolled participants.
Conclusion. Primary results for the C3FIT trial will be presented. Post-stroke, patients face continued risk for decreased cognitive/physical disability and quality of life. C3FIT’s results may contribute to improved post-stroke care.
More abstracts on this topic:
Application of Digital Health Interventions in Quality of Life and Psychological Status of Stroke Patients: Systematic Review and Meta-analysis
Chen Lu, Shang Zhiying, He Manlan
Computed Tomography Perfusion Imaging Profiles Are Similar Before and After Transfer to a Comprehensive Stroke Center.Oostema John, Wideman Brian, Abobaker Esam, Miller Malgorzata, Khan Nadeem, Khan Muhib, Reeves Mathew
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)