Final ID: TP4
Characterization of Acute Ischemic Stroke (AIS) patients excluded from thrombolysis due to recent NOAC use.
Methods: The GWTG database was queried for patients with acute ischemic stroke presenting (time frame) within 4.5 of last known well. A total of 1,933 AIS patients were identified). A total of 5.0 % (n=96) of these patients were excluded due to recent NOAC use. A chi-squared analysis was performed to determine if there was a significant difference based on sex, race, age, history of heart disease and statin use. A pooled T-test analysis was also performed to determine if a significant difference exists between the mRS and NIHSS at baseline and at discharge within the excluded patients group.
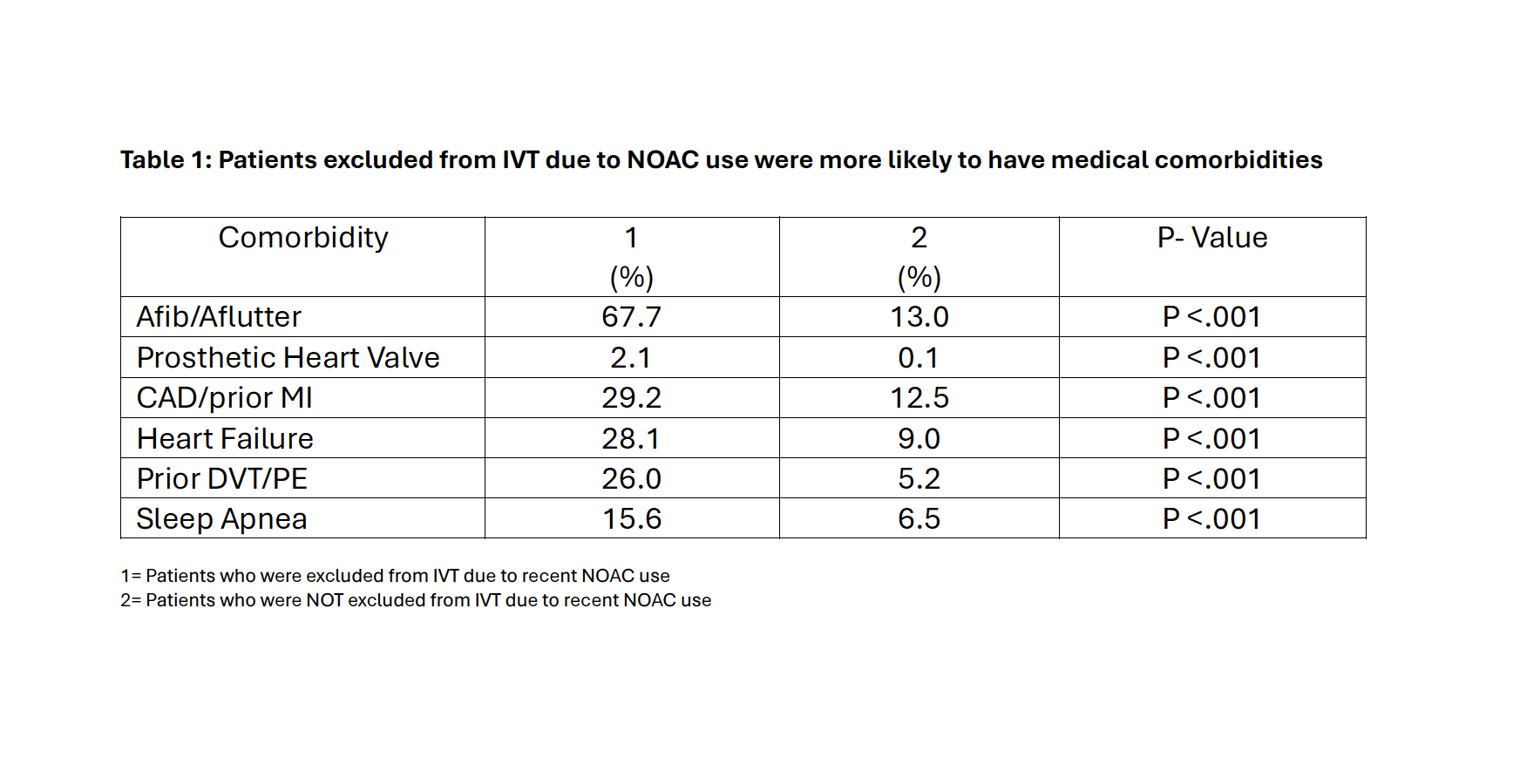
Results: Patients excluded from IVT due to recent NOAC use were more likely to take cholesterol reducer (67.1% vs 45.6%). The NOAC exclusion group were more likely to have medical co-morbidities including Afib/Aflutter, prosthetic heart valves, CAD/prior MI, heart failure, prior DVT/PE and sleep apnea (Table 1). Both groups had an equal probability of having a history of a previous stroke. There was no statistically significant difference in patient demographics (race, sex,etc.) between the two groups.
Among the patients excluded from IVT due to recent NOAC use: 54.2% (n=52) had a normal EF, 10.8 % (n=10) had a thrombus visualized on TTE, 49.0 % (n=47) had a L.MCA stroke. 80.2% (n=77) had plans to restart their AC on discharge: Apixaban 45.8% (n=44), Rivaroxaban 11.5% (n=11) and Dabigatran 2.1 % (n=11). The median mRS at baseline was 1 and at discharge was 4.
Conclusion: Patients excluded from IVT due to recent NOAC use were more likely to have cardiovascular co-morbidities. If NOAC exclusion is removed in the future, 1 in 20 patients could potentially become eligible for IVT, and MRS worsening due to stroke can potentially be avoided.
More abstracts on this topic:
Ramalingam Archana, Shabnam Arshiya, Devi Reddy Akhila Reddy, Nookala Vinod
Bleeding with the FXI Inhibitor Abelacimab compared with Rivaroxaban in Patients on Antiplatelet therapy: A Prespecified Analysis of the AZALEA-TIMI 71 TrialAl Said Samer, Goodman Shaun, Joung Boyoung, Kiss Robert, Spinar Jindrich, Wojakowski Wojciech, Weitz Jeffrey, Bloomfield Dan, Sabatine Marc, Ruff Christian, Patel Siddharth, Giugliano Robert, Morrow David, Goodrich Erica, Murphy Sabina, Hug Bruce, Parker Sanobar, Chen Shih-ann
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.