Final ID: TMP81
Endovascular Thrombectomy Outcomes in Acute Ischemic Stroke With Oral Anticoagulation Use: Secondary Analysis From the SELECT Study
Abstract Body: Introduction: Using oral anticoagulation (OAC) at baseline is hypothesized to increase the risk of hemorrhagic transformation after endovascular thrombectomy (EVT). However, several prior studies evaluating EVT in patients on OAC demonstrated conflicting results regarding functional and safety outcomes. We aimed to characterize the association between baseline use of OAC and EVT outcomes from SELECT, a multicenter, prospective cohort study.
Methods: From SELECT study, patients with acute ischemic stroke and large vessel occlusion within 24 hours from onset who received EVT were identified. Patients were stratified based on baseline OAC use, and their clinical and imaging characteristics and functional and safety outcomes were described and compared.
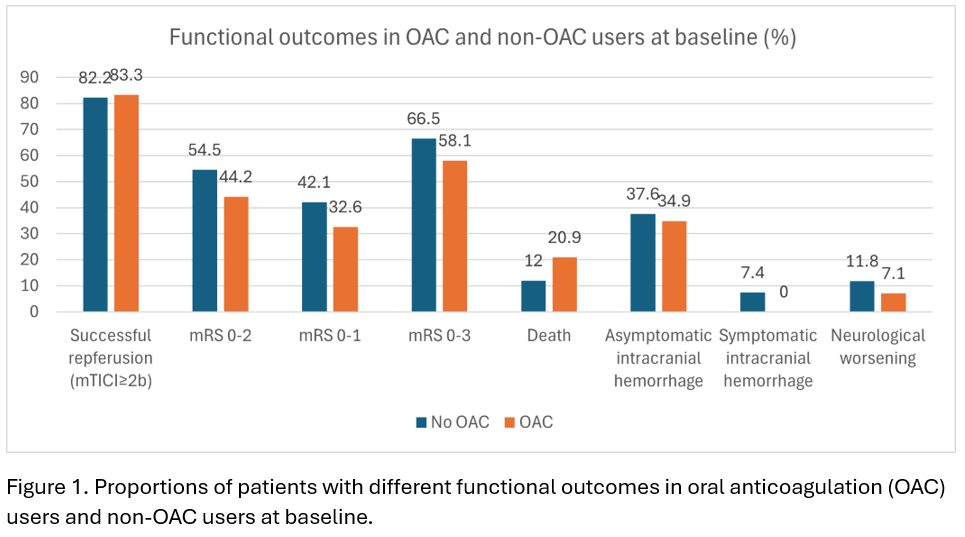
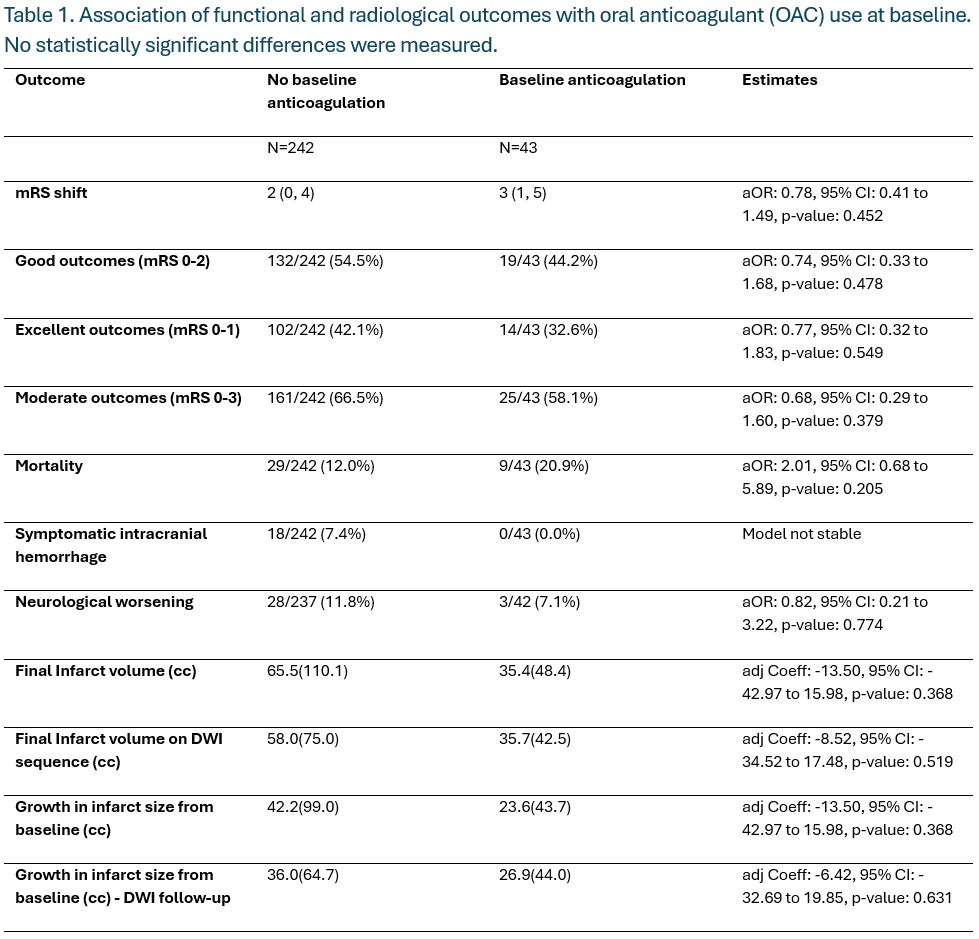
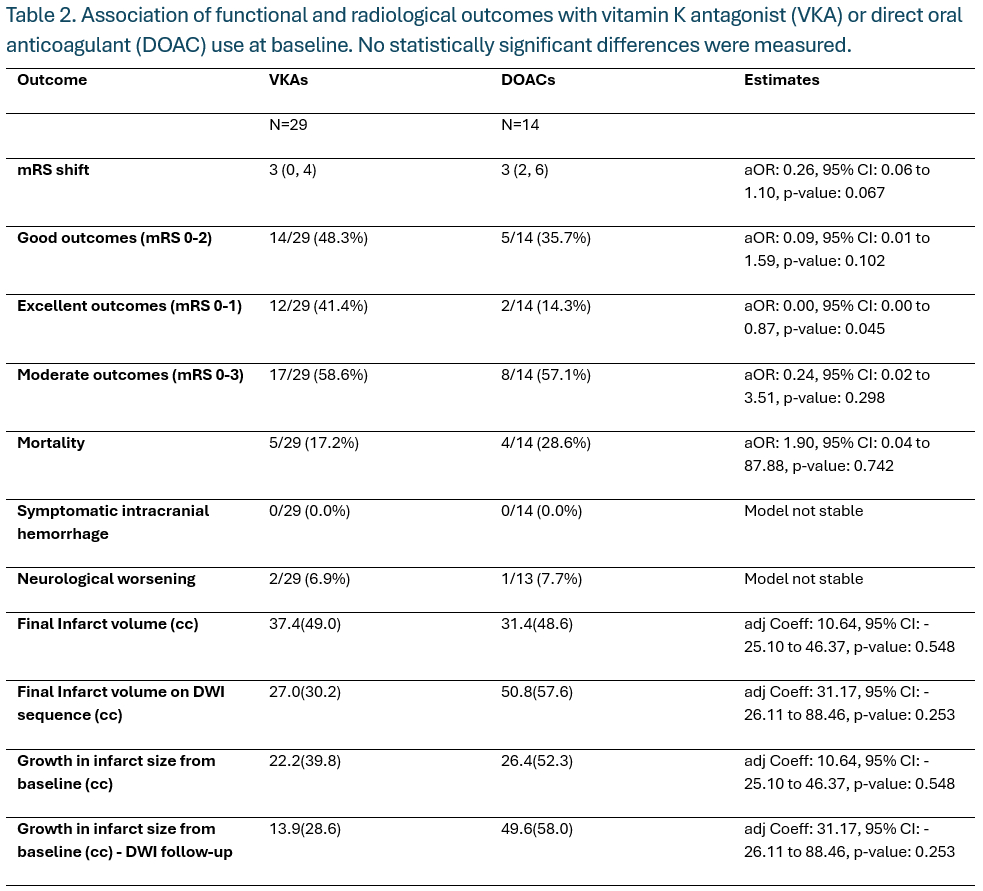
Results: Forty-three (15%) out of 285 patients used OAC at baseline, 29 (10%) were on vitamin K antagonists (VKA), and 14 (5%) were on direct oral anticoagulants (DOAC). OAC users were older (median age 75 years old vs 65) and had higher comorbidities - hypertension (88.4% vs 71.3%), diabetes mellitus (41.9% vs 25.7%), atrial fibrillation (64.3% vs 28.2%), and congestive heart failure (23.8% vs 9.6%), had smaller ischemic core volume at baseline (median [IQR]: 0cc [0-12] vs 11cc [0-32][SS1] ), and received alteplase less often (46.5% vs 69.0%, P <0.05 for all). OAC use was not significantly associated with worse clinical outcomes such as functional independence (modified Rankin Scale 0-2, OAC 44.2%, no OAC 54.5%, aOR 0.74, 95% CI: 0.33 to 1.68, p-value: 0.48) [SS2] [SS3] and mortality (OAC 20.9%, no OAC 12.0%, aOR 2.01, 5% CI: 0.68 to 5.89, p-value: 0.21); no OAC users had symptomatic intracranial hemorrhage (figure 1, table 1). There were no statistically significant differences between VKA vs DOAC users, including functional independence (48.3% vs 35.7%, aOR: 0.09, 95% CI: 0.01 to 1.59) and mortality (17.2% vs 28.6%, aOR: 1.90, 95% CI: 0.04 to 87.88; P >0.05 for both; table 2).
Conclusion: Almost 1 in 7 patients receiving EVT had baseline use of OACs, with higher comorbidities. OAC use at baseline was not associated with poor functional outcomes. We also did not observe symptomatic intracranial hemorrhage among EVT patients with baseline OAC use, suggesting limited safety concerns due to hemorrhagic transformation. There was no difference in outcome between VKA users and DOAC users.
Methods: From SELECT study, patients with acute ischemic stroke and large vessel occlusion within 24 hours from onset who received EVT were identified. Patients were stratified based on baseline OAC use, and their clinical and imaging characteristics and functional and safety outcomes were described and compared.
Results: Forty-three (15%) out of 285 patients used OAC at baseline, 29 (10%) were on vitamin K antagonists (VKA), and 14 (5%) were on direct oral anticoagulants (DOAC). OAC users were older (median age 75 years old vs 65) and had higher comorbidities - hypertension (88.4% vs 71.3%), diabetes mellitus (41.9% vs 25.7%), atrial fibrillation (64.3% vs 28.2%), and congestive heart failure (23.8% vs 9.6%), had smaller ischemic core volume at baseline (median [IQR]: 0cc [0-12] vs 11cc [0-32][SS1] ), and received alteplase less often (46.5% vs 69.0%, P <0.05 for all). OAC use was not significantly associated with worse clinical outcomes such as functional independence (modified Rankin Scale 0-2, OAC 44.2%, no OAC 54.5%, aOR 0.74, 95% CI: 0.33 to 1.68, p-value: 0.48) [SS2] [SS3] and mortality (OAC 20.9%, no OAC 12.0%, aOR 2.01, 5% CI: 0.68 to 5.89, p-value: 0.21); no OAC users had symptomatic intracranial hemorrhage (figure 1, table 1). There were no statistically significant differences between VKA vs DOAC users, including functional independence (48.3% vs 35.7%, aOR: 0.09, 95% CI: 0.01 to 1.59) and mortality (17.2% vs 28.6%, aOR: 1.90, 95% CI: 0.04 to 87.88; P >0.05 for both; table 2).
Conclusion: Almost 1 in 7 patients receiving EVT had baseline use of OACs, with higher comorbidities. OAC use at baseline was not associated with poor functional outcomes. We also did not observe symptomatic intracranial hemorrhage among EVT patients with baseline OAC use, suggesting limited safety concerns due to hemorrhagic transformation. There was no difference in outcome between VKA users and DOAC users.
More abstracts on this topic:
A Multi-Center Clinic Site Comparison of Patient-level factors Affecting Oral Anticoagulation Prescription for Atrial Fibrillation
Iqbal Fatima, Hoang Kenneth, Chiadika Simbo
A Case Series of Papillary Fibroelastomas on the Coumadin ridgeAboukhatwa Omar, Akiki Elias, Kurmann Reto, Larson Kathryn, Keeney Michael, Bois Melanie, Klarich Kyle
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)