Final ID: WMP76
Trends in ischemic stroke hospitalization and outcomes in the United States pre- and peri- COVID-19 pandemic: A National Inpatient Sample study
Objective: To evaluate the impact of the COVID-19 pandemic on AIS admissions, treatment utilization, complications & outcomes in the U.S. from 2016 to 2021, focusing on the pre-pandemic (2016-2019) & peri-pandemic (2020-2021) periods.
Methods: A retrospective observational cohort study utilizing the National Inpatient Sample (NIS) nationwide database, analyzing weighted hospital discharge records over 6 years, encompassing urban, rural, teaching &non-teaching hospitals.
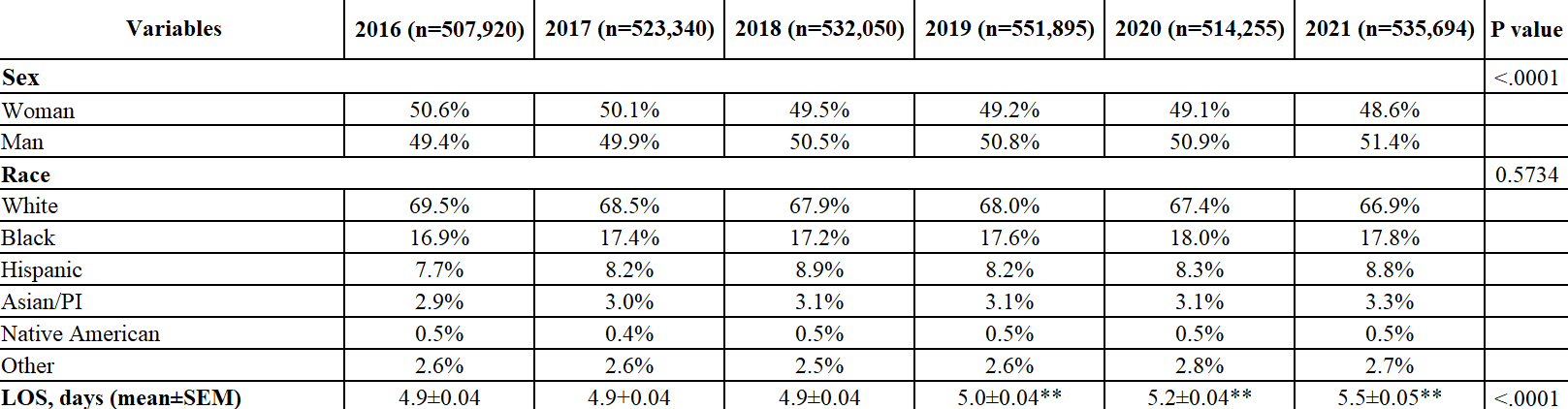
Participants were AIS patients aged 18 years & older (n=3,154,154), identified using ICD-10 codes. Sociodemographic characteristics such as age, sex, race & comorbidities were evaluated. The mean patient age was 70.0 ± 0.03 years, with an average length of stay of 5.1 ± 0.01 days & an adjusted mean cost of $16,765 ± 71. Men accounted for 50.5% of the cohort. AIS hospitalizations from 2016 to 2021 were collected, comparing pre- & peri-pandemic periods. Primary outcomes included AIS admission trends, while secondary outcomes included reperfusion therapy utilization, intubation & ventilation rates, discharge disposition & complications.
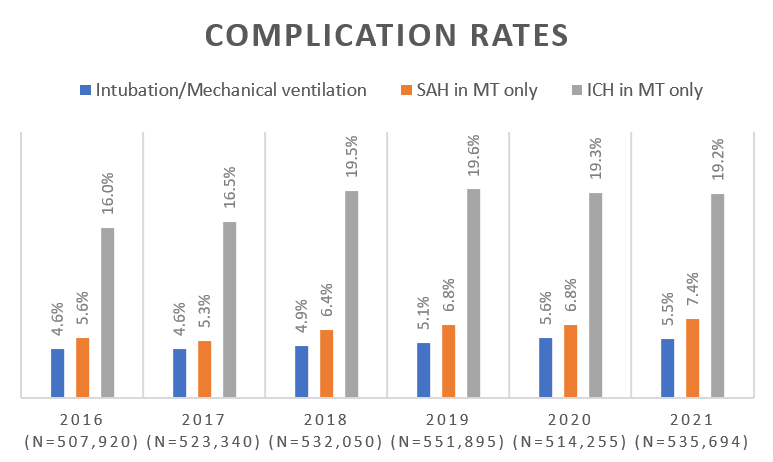
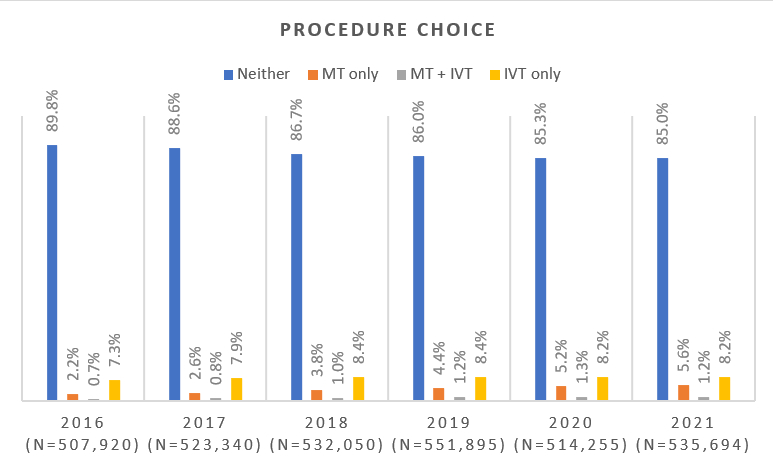
Results: AIS admissions increased from 507,920 in 2016 to 535,694 in 2021. A demographic shift was observed, with the proportion of male patients rising from 49.8% to 51.4% & the mean age decreasing from 70.3 to 69.7 years (p < 0.0001). Most patients were White (69.5% in 2016), but their proportion decreased over time, while Black, Hispanic & Asian/Pacific Islander cases increased (p 0.5734). Reperfusion therapy usage increased, with mechanical thrombectomy (MT) rising from 2.2% to 5.6% in 6 years. Intubation/ventilation rates grew from 4.8% pre-COVID to 5.5% peri-COVID (p < 0.0001). Subarachnoid & intracerebral hemorrhage rates had increased throughout the 6 years in the group with MT-only intervention (p .011 & .002, respectively).
Conclusions: The COVID-19 pandemic led to significant shifts in AIS hospitalization patterns, including changes in age distribution, increased reperfusion therapy use & rising complications. These findings highlight the need for adaptive public health strategies & resource allocation to maintain stroke care during future crises.
More abstracts on this topic:
De Souza Abner Lucas, Reis Soares Filipe, Ventura Artur, De Vasconcelos Anna Victoria, Wagner Fernanda, Moro Izabela, Queiroz Ivo
ENHANCED FUNCTIONAL OUTCOMES WITH BRIDGING THROMBOLYSIS BEFORE ENDOVASCULAR THERAPY IN LARGE CORE STROKE WITHIN 4.5 HOURS: A MULTICENTER OBSERVATIONAL STUDYLe Thien, Le Tra, Nguyen Nhi, Dang Hung, Pham Binh, Truong Anh, Nguyen-ba Thang, Nguyen Thang, Nguyen Trung, Nguyen Vinh Khang, Nguyen Son, Tran Hang, Nguyen Huong, Nguyen Lanh, Bach Dung, Phan Bang
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.