Final ID: 72
ENHANCED FUNCTIONAL OUTCOMES WITH BRIDGING THROMBOLYSIS BEFORE ENDOVASCULAR THERAPY IN LARGE CORE STROKE WITHIN 4.5 HOURS: A MULTICENTER OBSERVATIONAL STUDY
Numerous clinical trials have established that bridging therapy with intravenous thrombolysis before endovascular therapy (EVT) is the standard treatment for acute ischemic stroke with large vessel occlusion (AIS-LVO) patients. However, the benefit of bridging therapy in patients with acute large ischemic core (LIC) remains unclear. We hypothesize that compared with EVT alone, bridging therapy may be associated with improved functional outcomes and higher reperfusion rates.
Methods
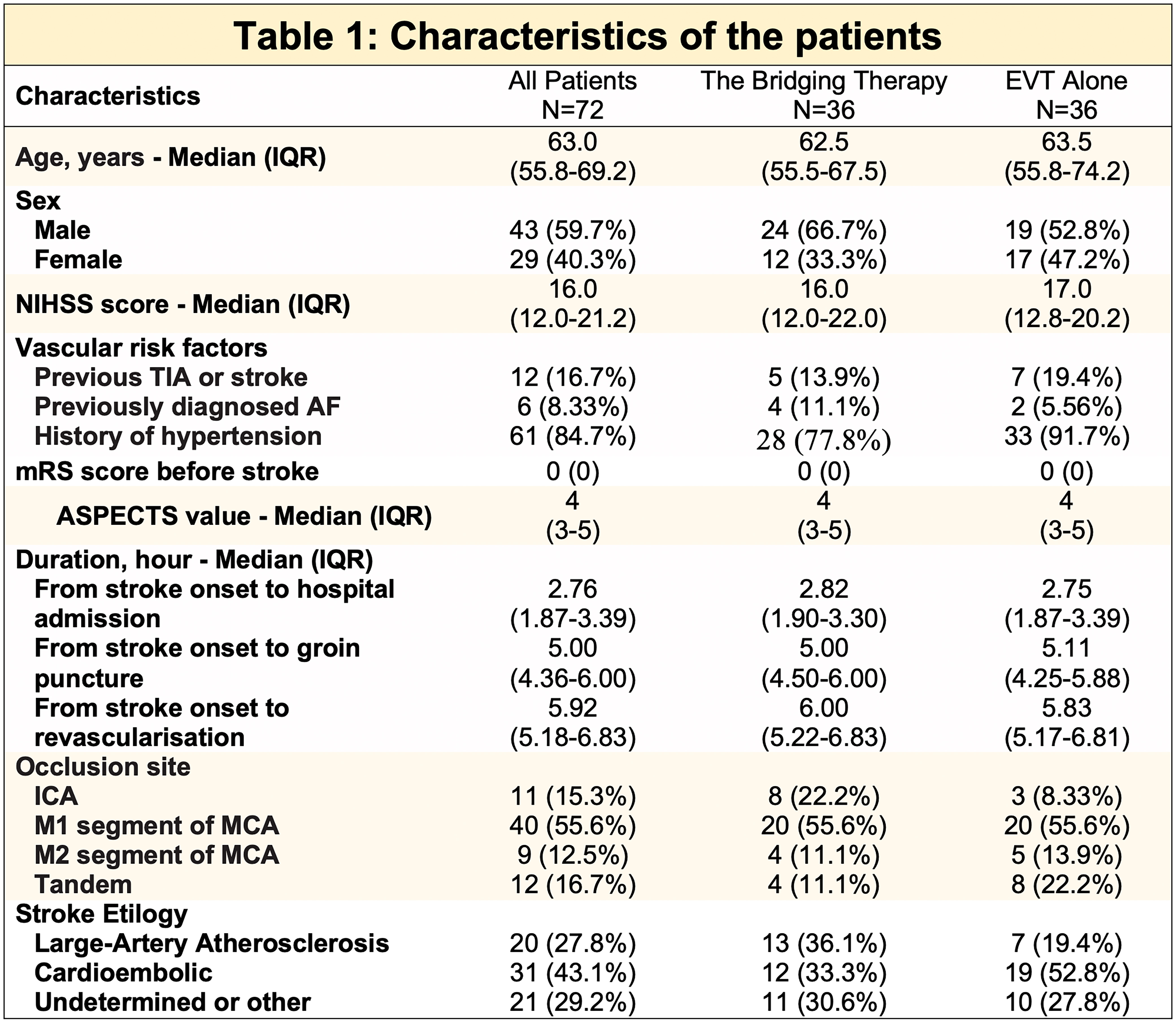
A prospective, multicenter, observational study was conducted at 4 stroke centers in Vietnam between August 2023 and June 2024. We enrolled patients with AIS-LVO in the anterior circulation within 4.5 hours of onset, an Alberta Stroke Program Early CT Score (ASPECTS)< 6, and a National Institutes of Health Stroke Scale (NIHSS) ≥ 6 at admission. Short-term favorable outcomes were defined as a modified Rankin scale of 0 to 2 at 30 days. Safety outcomes were defined by symptomatic intracranial hemorrhage (ICH) according to SITS-MOST criteria and 30-day mortality. We defined successful recanalization with a modified Thrombolysis In Cerebral Infarction scale of 2b-3. Outcomes between the bridging therapy and EVT alone groups were compared using propensity score-matched (PSM) analysis.
Results
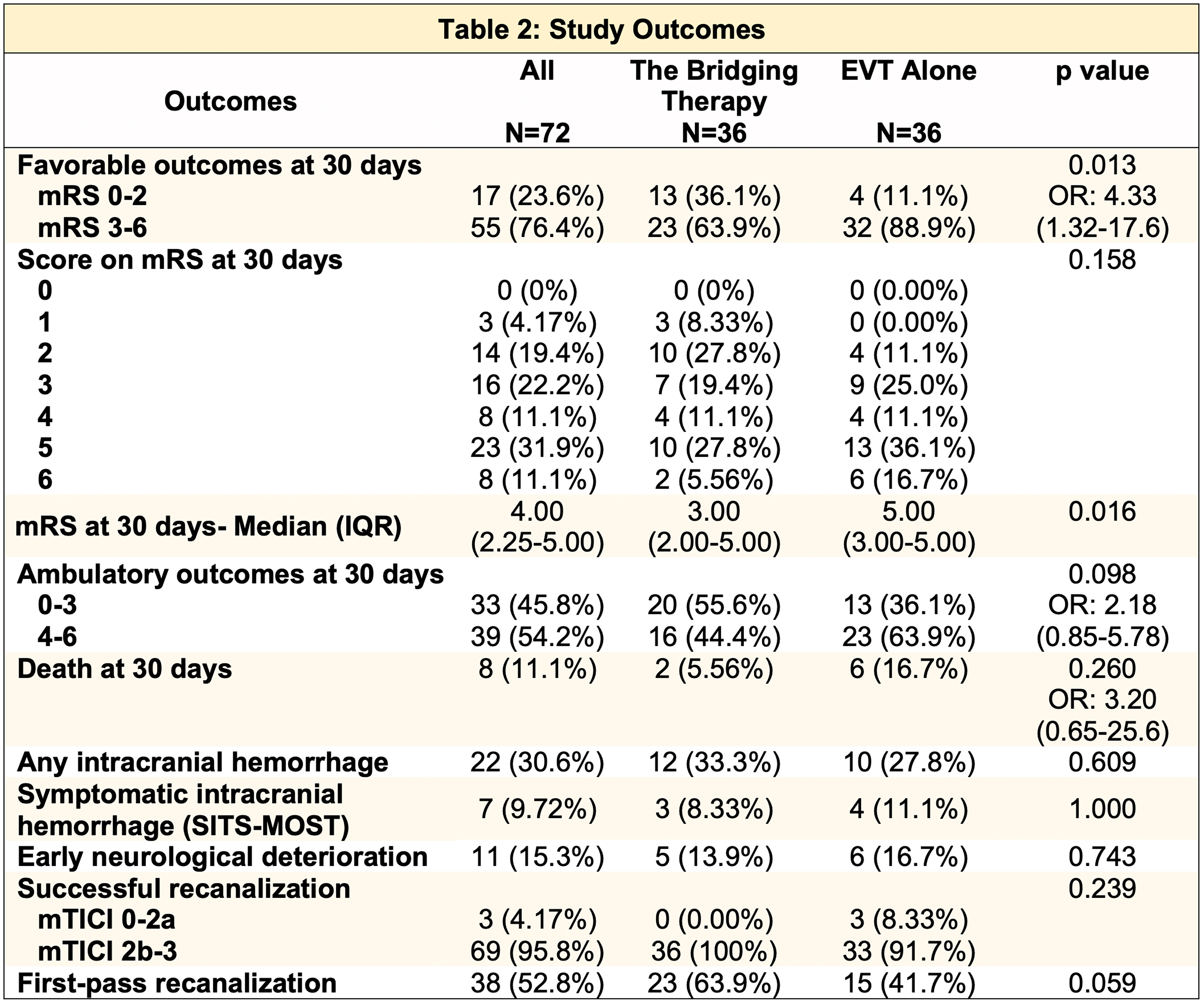
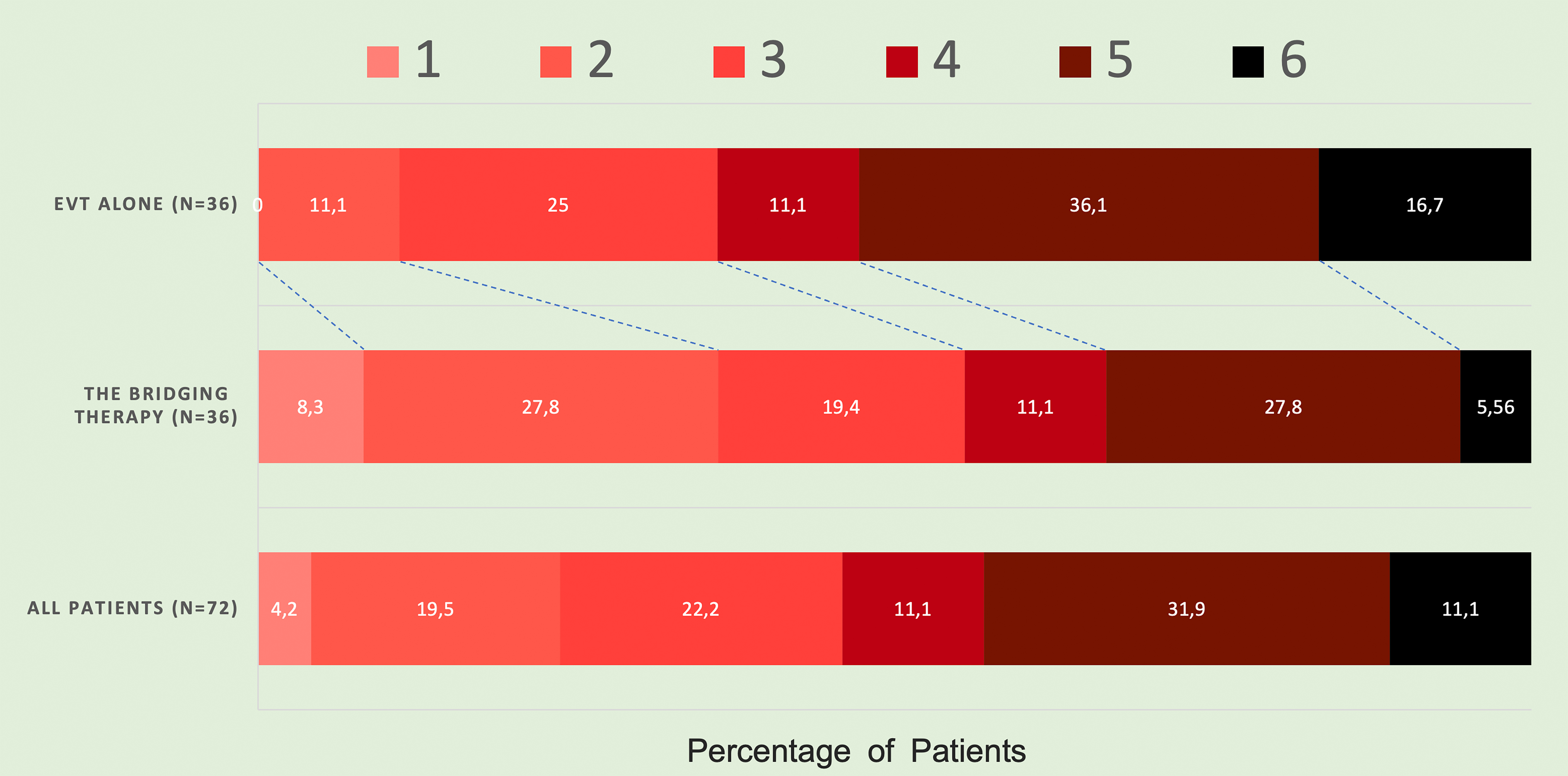
We screened 407 patients with LIC thrombectomy; 148 patients(36.7%) were admitted within 4,5 hours of onset. After PSM, we analyzed 72 patients, with 36 in each group. The median age was 63, and 59.7% of the patients were men. Baseline ASPECTS was 4 (IQR: 3–5), and NIHSS was 16 (IQR: 12.0–21.2). Compared with EVT alone, the bridging therapy groups showed a higher rate of favorable outcome rate at 30 days (36.1% vs. 11.1%, p=0.013), with numerically lower mortality (5.56% vs. 16.7%, p=0.26). The rate of any ICH was higher in the bridging group (33.3% vs. 27.8%, p=0,609), but there was no significant between-group difference in the frequency of symptomatic ICH (8.33% vs.16%; p=0,11). The bridging therapy group had higher successful recanalization rates (100% vs. 91.7%, p=0.239) and first-pass recanalization rates (63.9% vs. 41.7%, p=0.059) than EVT alone.
Conclusions
This study’s findings suggest that bridging therapy in patients with acute large ischemic core within 4.5 hours of onset results in better functional outcomes and recanalization efficacy than EVT alone without increasing the sICH rate. Further studies are required to assess the safety and efficacy of bridging therapy.
More abstracts on this topic:
Thomas Tarun, Tonetti Daniel, Shaikh Hamza, Jovin Tudor, Koneru Manisha, Dubinski Michael, Patel Karan, Penckofer Mary, Khalife Jane, Thon Jesse, Schumacher Hermann, Hanafy Khalid, Patel Pratit
A Novel Imaging Biomarker to Make Precise Outcome Predictions for Patients with Acute Ischemic StrokeMallavarapu Monica, Kim Hyun Woo, Iyyangar Ananya, Salazar-marioni Sergio, Yoo Albert, Giancardo Luca, Sheth Sunil, Jeevarajan Jerome