Final ID: TP278
Final infarct volume reduction may mediate EVT effects on mortality
Methods: From our prospectively collected multi-center registry across four comprehensive stroke centers (CSC) in the Houston area, we identified patients from 2017 to 2023 with large vessel occlusion acute ischemic stroke (LVO AIS) who underwent thrombectomy. A large infarct core was defined by CTP as exceeding 70 ml or by CT ASPECTS < 6. This study conducted a mediation analysis to investigate the relationship between EVT (independent variable), 90-day mortality (outcome), and FIV (mediator). Bootstrapping was used to estimate indirect effect, adjusting for confounders, including age and sex. Separate mediation analyses were performed for severe and non-severe subgroups.
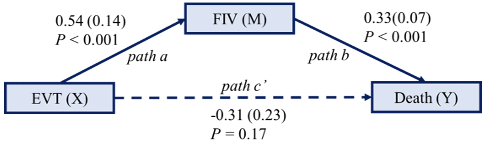
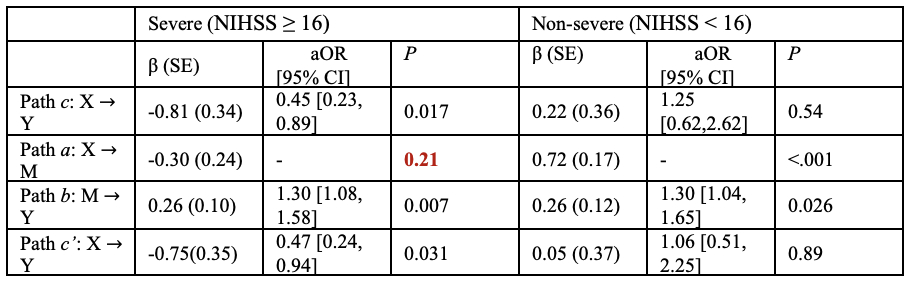
Results: Among 616 patients with LVO AIS who underwent EVT, median NIHSS was 14 [8,20 IQR], age was 67 [57,77 IQR] and 47.2% were female. Median FIV was 20.38 [ 4.26, 60.20 IQR] and 19.2 % of patients suffered mortality. In the overall cohort, the total effect of EVT on 90-day mortality was not statistically significant (P = 0.46 unadjusted; P = 0.68 adjusted). EVT significantly influenced FIV with a P-value < 0.001, and FIV was a strong predictor of mortality with a P-value < 0.001. However, when accounting for FIV, the direct effect of EVT on mortality was not significant (P = 0.17 unadjusted; P = 0.31 adjusted). The impact of EVT on 90-day mortality was partially mediated via FIV. The indirect effect of EVT on mortality through FIV was significant (P < 0.001). Subgroup analyses indicated that in severe stroke patients (NIHSS ≥ 16), EVT did not significantly affect FIV (Path A, P = 0.21), precluding mediation analysis. In non-severe stroke patients (NIHSS < 16), EVT had a significant impact on FIV (P < 0.001), and FIV was a significant predictor of mortality (P = 0.026). In this group, 77.7% of EVT’s effect on mortality was mediated by FIV.
Conclusions: Reductions in FIV partially mediate the effect of EVT on 90-day mortality, particularly in patients with NIHSS < 16. These findings support the results of recent clinical trials demonstrating mortality benefit with reperfusion.
More abstracts on this topic:
Perera Sudheesha, Wadhera Rishi, Khullar Dhruv
Association of Workflow Metrics with Functional Outcomes in the SELECT2 trialJabbour Pascal, Sitton Clark, Churilov Leonid, Hill Michael, Ribo Marc, Campbell Bruce, Gandhi Chirag, Tjoumakaris Stavropoula, Sarraj Amrou, Al-mufti Fawaz, Hassan Ameer, Abraham Michael, Hussain Shazam, Ortega-gutierrez Santiago, Chen Michael, Pujara Deep, Johns Hannah Tabitha
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.