Final ID: WP13
Determining Eligible Thrombolysis Candidates for Isolated Dizziness
Strokes affecting the posterior circulation (PCS) account for 20% of all ischemic strokes. In the emergency department, patients with PCS will often present with nonspecific symptoms such as dizziness, blurry vision, headache, nausea/vomiting, and altered mentation, leading to lower NIHSS scores. These also make PCS more prone to delayed recognition, missed diagnoses and delays in acute treatment. Recent studies indicate that PCS are half as likely to receive thrombolytic therapy and threefold less likely to receive intervention with mechanical thrombectomy compared to anterior circulation strokes (ACS). We aimed to create a protocol that identifies thrombolysis candidates for patients presenting with isolated dizziness.
Methods:
A code stroke activation protocol was implemented by the Rhode Island Hospital Stroke Committee in 08/2021. In addition to focal neurological symptoms typically associated with ACS, the protocol included objective criteria for a chief complaint of sustained isolated dizziness, including evidence of localizing examination findings and <24 hrs since last known well (LKW), or new balance issues and <4.5 hrs since LKW. A retrospective chart review was conducted for patients between 01/2021-06/2024 with a chief complaint of isolated dizziness. We compared the patients’ discharge diagnoses, decision for thrombolytic administration, door to activation times, and door to needle times.
Results:
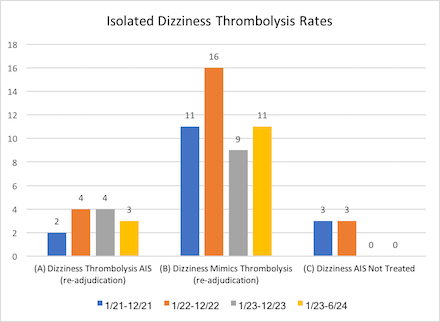
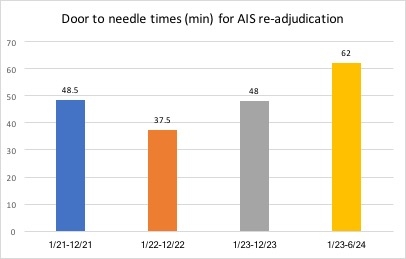
In the years 2021 and 2022, there were 3 missed thrombolysis opportunities per year for patients presenting with isolated dizziness. From 01/2023-06/2024 there were 0 misses. The number of stroke mimics presenting with isolated dizziness who received thrombolysis was 11 in 2021, 16 in 2022, 9 in 2023, and 11 in 2024. The average door to needle time (in min) for patients with isolated dizziness and a diagnosis of acute ischemic stroke were 48.5 in 2021, 37.5 in 2022, 48 in 2023, and 62 in 2024. All delays in door to needle times were related to delayed activation, though all cases should have met criteria for the protocol.
Conclusion:
A simplified protocol is feasible to identify stroke patients with isolated dizziness eligible for thrombolysis. Use of the protocol reduced the number of missed PCS, however it also increased the number of stroke mimic patients who received thrombolysis for isolated dizziness. Continued education of the protocol is required to reduce the door to needle times in patients with isolated dizziness.
More abstracts on this topic:
Ferrone Nicholas, Sanmartin Maria, O'hara Joseph, Jimenez Jean, Ferrone Sophia, Wang Jason, Katz Jeffrey, Sanelli Pina
A machine learning approach to classifying ischemic stroke etiology using variables available in the Get-with-the-Guidelines Stroke RegistryLee Ho-joon, Schwamm Lee, Turner Ashby, De Havenon Adam, Kamel Hooman, Brandt Cynthia, Zhao Hongyu, Krumholz Harlan, Sharma Richa
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.