Final ID: WP106
Bridging the Gap: System of Care Partnerships to Improve Prehospital Diagnostic Error
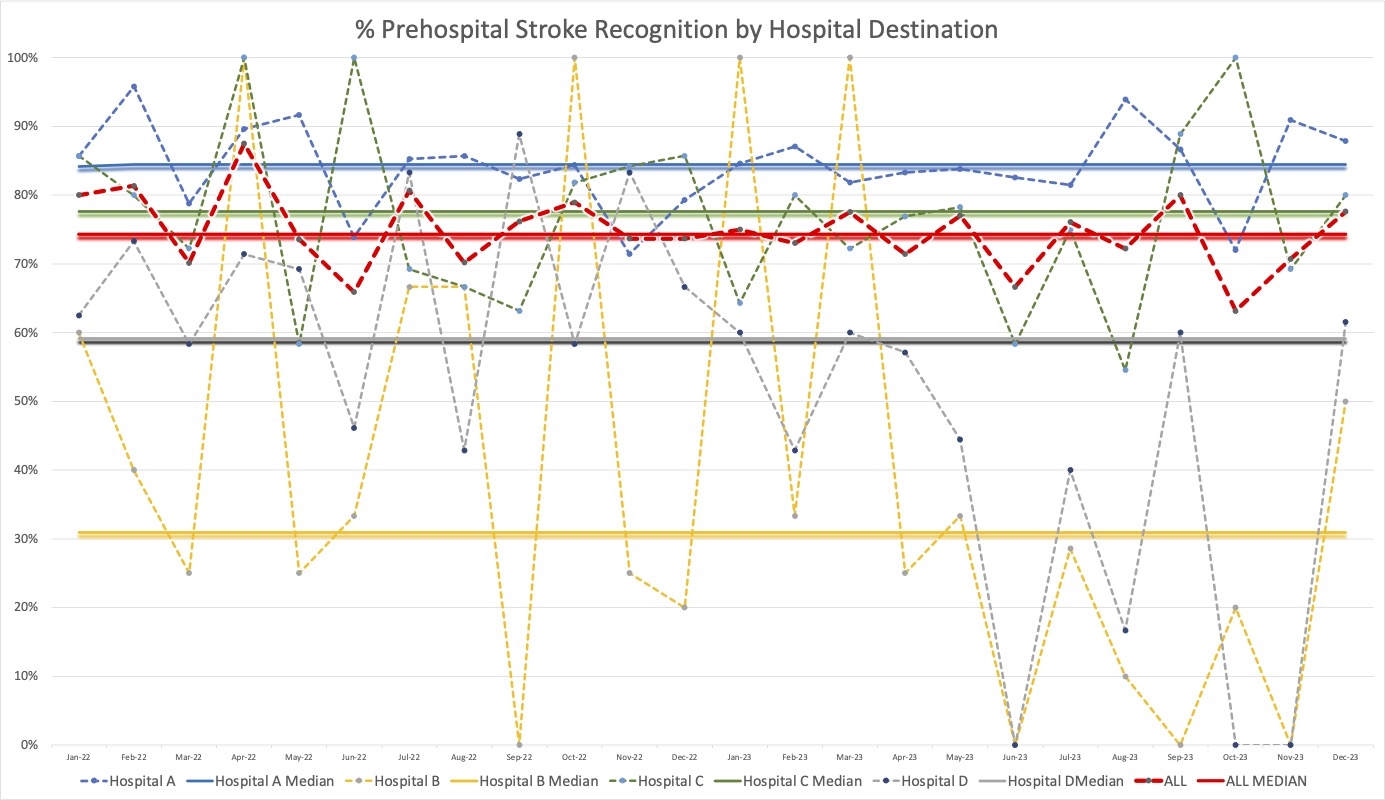
Abstract Body: Introduction: Emergency Medical Services (EMS) play a key role in stroke systems of care. Prehospital stroke recognition is critical, but limited data exchange between prehospital and hospital entities hinders the ability to measure and improve this aspect of stroke care. To measure baseline prehospital stroke recognition and inform quality improvement efforts, we developed a regional collaboration for sharing Get with the Guidelines (GTWG) data with regional EMS leadership. Methods: This was a retrospective analysis of GWTG registry data from all hospitals in a single county, including two comprehensive stroke centers (CSC) and two primary stroke centers (PSC) spanning two health systems for quality improvement. Patients were included if they had a diagnosis of ischemic stroke, developed stroke symptoms before hospital admission and arrived by EMS. Percent prehospital stroke recognition was measured across all hospitals. A subset of missed strokes were analyzed for dispatch code, primary impression and assessments performed. Results: In 2022-23,1848 ischemic stroke patients were transported by EMS to four hospitals in a single county. 17%(348) of GWTG entries were missing prehospital information and excluded from analysis. Amongst the remaining 1503 patients, stroke was recognized prehospital 75% of the time. Prehospital stroke recognition varied by destination hospital with CSCs having the highest prehospital stroke recognition. Missed strokes brought to one PSC were reviewed to identify common themes. The most common primary impressions were Generalized Weakness (39%), Fall (15%), Altered Mental Status (15%), Nausea/Vomiting (10%) and Dizziness (10%). 41% of patients had a prehospital stroke scale documented (CPSS). The most common prehospital dispatch codes were stroke (23%), fall (16%) and generalized illness (16%). Missed strokes were predominantly localized to the posterior (57%) and frontal (20%) regions. Results have been used to develop regional symptom-based EMS care bundles, standardize EMS feedback, and inform initial and continuing education for EMS clinicians. Conclusion: Prehospital stroke recognition varies greatly between destination hospitals with PSCs more likely to receive patients with prehospital diagnostic error. Measuring and improving prehospital stroke recognition requires a regional approach involving bidirectional information sharing and collaboration between hospitals, health systems, and regional EMS leadership.
More abstracts on this topic:
A Hospital-Wide Multidimensional Approach to Pediatric In-Hospital Cardiac Arrest Review: Early Identification and Prevention
Loeb Daniel, Collins Kelly, Ortega Karina, Dewan Maya
Acoustic Biomarkers Harvested from 911 Calls Differ among Patients with Cardiac and Non-Cardiac Chest PainMazhar Harris, Zegre-hemsey Jessica, Lee Kyungbok, Tian Baotong, Heydari Mojtaba, Cushman Jeremy, Duan Zhiyao, Dzikowicz Dillon
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)