Final ID: TP203
Effects of Cyclooxygenase Inhibitors on Patients with Acute Intracerebral Hemorrhage
Methods: This study retrospectively enrolled patients with acute ICH hospitalized in our Hospital between Jan. 2015 and Dec. 2020. The exclusion criteria were delayed hospitalization for more than 10 days, transferal to other hospital within 10 days, ICH etiologies as trauma, structural lesion, medication, or systemic diseases. Although aspirin belongs to COXi, aspirin users were excluded because of the antiplatelet effect. Patients with continuous usage of COXi for at least three days were defined as COXi users. The effects of using COXi before or after ICH were analyzed individually. Good functional outcome was defined as modified Rankin Scale score 0-2 at 3 months.
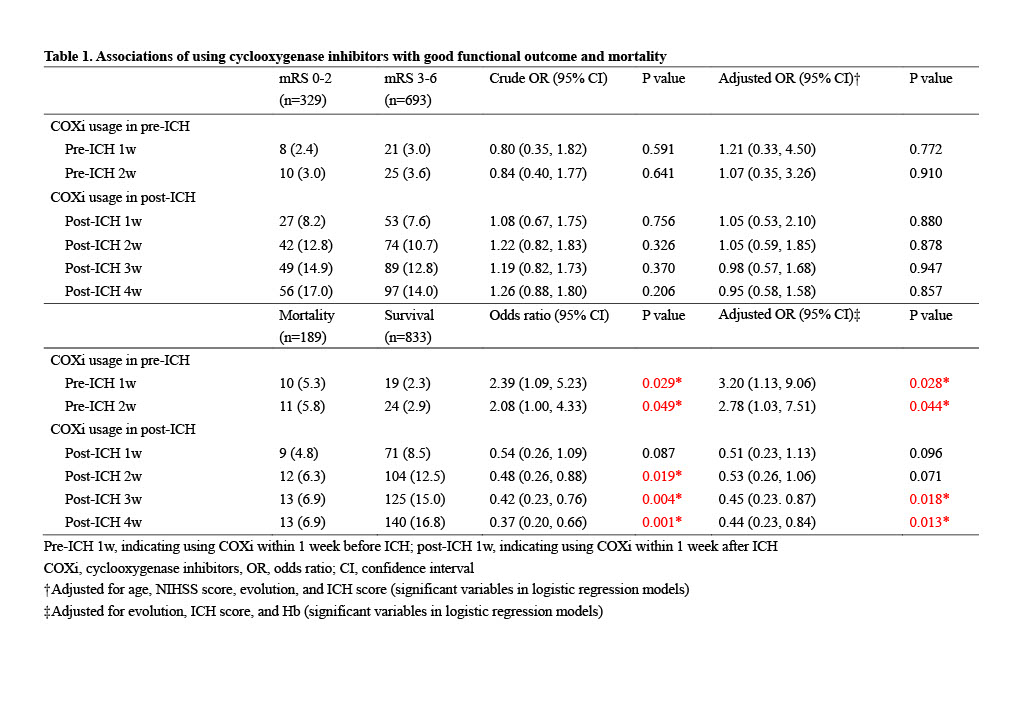
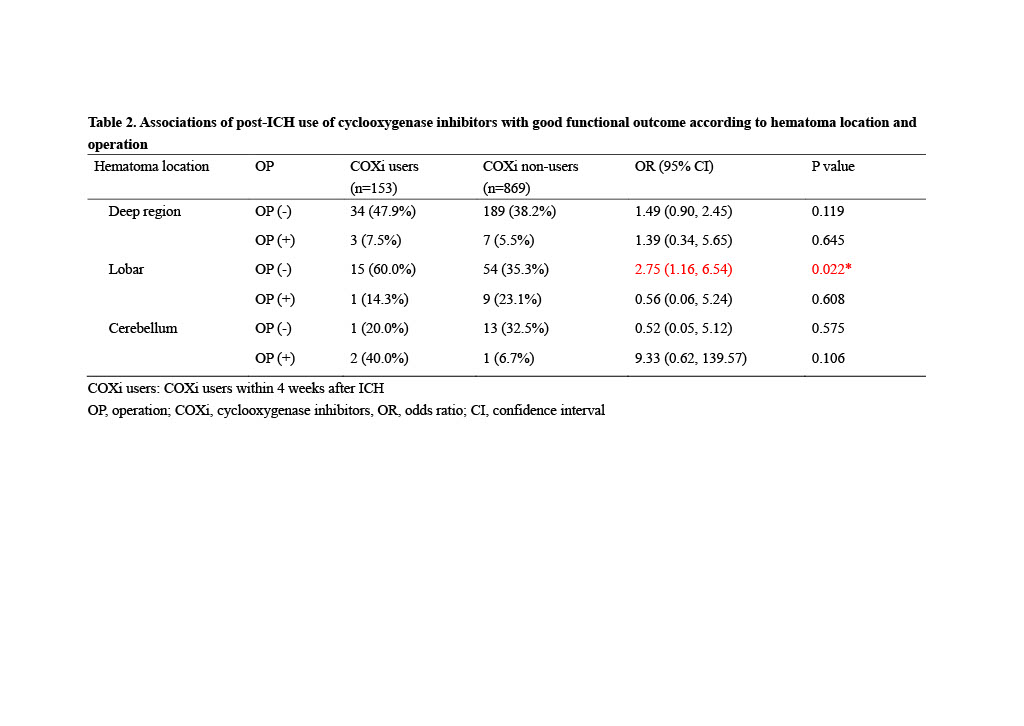
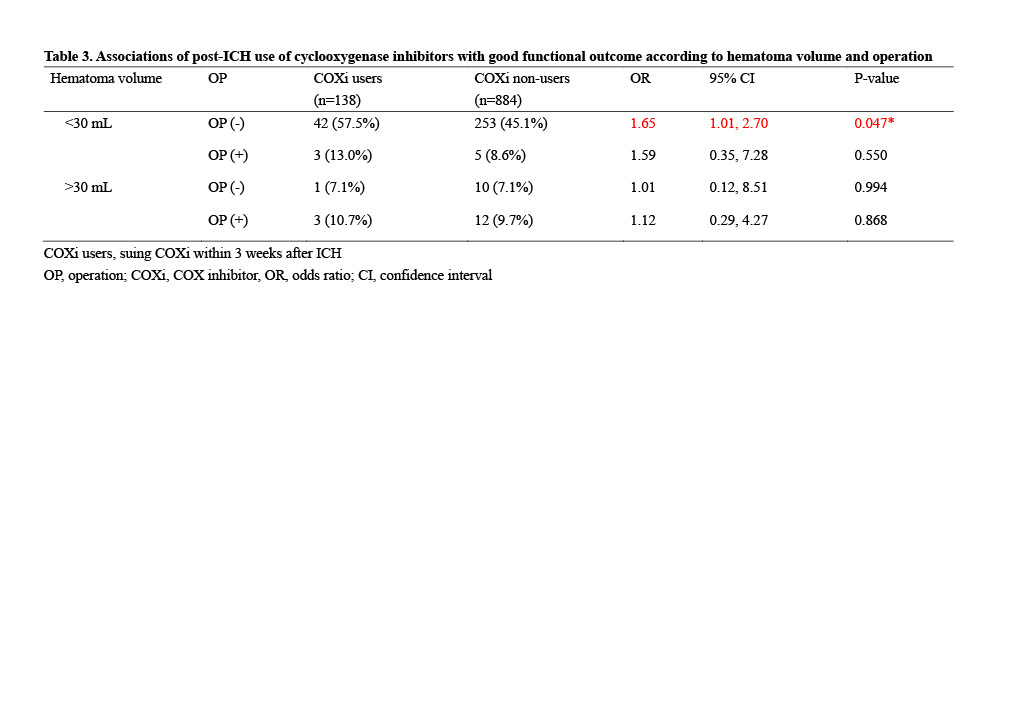
Results: A total of 1,022 patients were enrolled, in whom 35 (3.4%) used COXi within 2 weeks before ICH while 154 (15.1%) used COXi within 4 weeks after ICH. Patients using COXi before ICH were older, had a lower hemoglobin level, and more lobar hematoma. Patients using COXi after ICH were younger, had a lower NIHSS score, and higher percentage of operation. In multivariate logistic regression models, using COXi before ICH was associated with a higher mortality risk [using within 1 week: adjusted odds ratio (aOR) 3.20, 95% CI (1.13, 9.06), p = 0.028; within 2 weeks, aOR 2.78, 95% CI (1.03, 7.51), p = 0.044]. On the contrary, using COXi after ICH was associated with a lower mortality risk [using within 3 weeks: aOR 0.45, 95% CI (0.23. 0.87), p = 0.018; within 4 weeks, aOR 0.44, 95% CI (0.23, 0.84), p = 0.013]. The usage of COXi after ICH was associated with a good functional outcome specifically in patients with a non-operated lobar hematoma [OR 2.75, 95% CI (1.16, 6.54), p = 0.022], and in those with a non-operated smaller hematoma (<30 mL) [OR 1.65, 95% CI (1.01, 2.70), p = 0.047]. Furthermore, ICH etiology of amyloid angiopathy was significantly associated with pre-ICH usage of COXi [aOR 2.90, 95% CI (1.36, 6.17), p = 0.006].
Conclusions: This study demonstrated different effects of COXi usage before and after ICH on long-term functional outcome and mortality in patients with acute ICH, specifically depending on hematoma location, volume, and operation.
More abstracts on this topic:
Abbasi Mohammad Hossein, Brensinger Colleen, Acton Emily, Favilla Christopher, Burkhardt Jan-karl, Kasner Scott
A Non-odorant Olfactory Receptor Ligand Depolymerizes the Platelet Actin Cytoskeleton to Prevent ThrombosisAggarwal Anu, Godwin Matthew, Ali Mariya, Jennings Courtney, Rajasekar Bhairavi, Scalise Alliefair, Stauffer Shaun, Mccrae Keith, Mcintyre Thomas, Cameron Scott, Wang Nancy, Josyula Vara Prasad, Yang Moua, Young Shim, Kennedy Quinn, Samuel Reina, Sangwan Naseer, Guntupalli Suman
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.