Final ID: WP282
Effectiveness and safety of apixaban vs. aspirin for primary prevention of stroke and bleeding risk among patients with atrial fibrillation: A Meta-analysis of randomized controlled trials including ARTESIA trial.
Abstract Body:
Background
Atrial fibrillation is a common arrhythmia that increases the risk of stroke. However, treatment of such patients with oral anticoagulants when compared with aspirin is not well established with uncertain benefits.
Objective
We analyzed available study level data comparing Apixaban and Aspirin for efficacy and safety among atrial fibrillation patients.
Methods
We performed a systematic literature search on PubMed, EMBASE, and ClinicalTrials.gov for relevant randomized controlled trials (RCTs) from inspection until August 10th, 2024, without any language restrictions. Odds ratios (OR) and 95% confidence intervals (CI) were pooled using a random-effect model, and a p-value of <0.05 was considered statistically significant.
Results
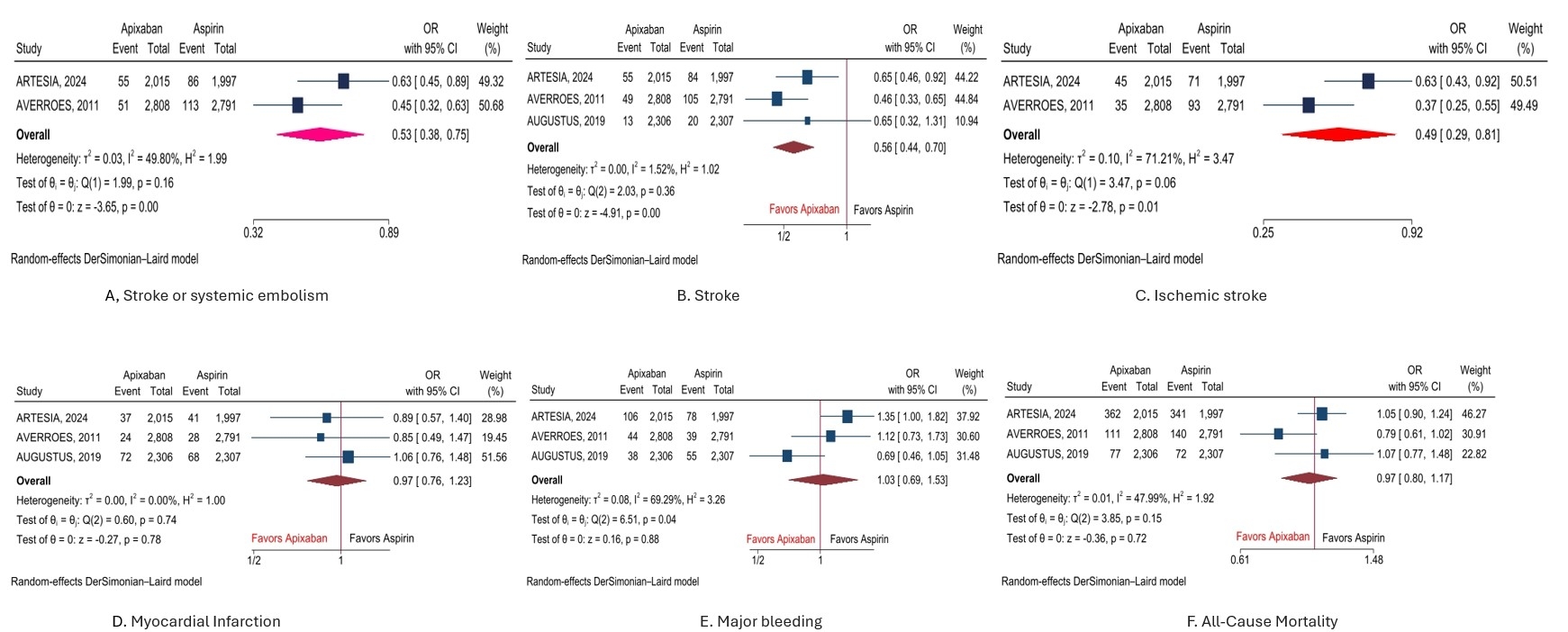
A total of 3 RCTs with 14,224 patients were included (7,129 in apixaban and 7095 in the aspirin group) in the analysis. The mean age of the patients in apixaban and the aspirin groups was 72.4 and 72.8 years, respectively. Pooled analysis of primary and secondary endpoints showed that apixaban significantly reduced the risk of stroke or systemic embolism by 47% (OR, 0.53(95%CI: 0.38-0.75), P<0.001), stroke by 44% (OR, 0.56(95%CI: 0.44-0.70), P<0.001), and ischemic stroke by 51% (OR, 0.49(95%CI: 0.29-0.81), P=0.01) when compared with aspirin. However, the risk of major bleeding (OR, 1.03(95%CI: 0.69-1.53), P=0.88), myocardial infarction (OR, 0.97(95%CI: 0.76-1.23), P=0.78), and all-cause mortality (OR, 0.97(95%CI: 0.80-1.17), P=0.72) was comparable when compared with the aspirin group of patients.
Conclusion
In this comprehensive analysis of randomized controlled trials data, the use of apixaban was associated with reduction in stroke or systemic embolism, and ischemic stroke, when compared with aspirin therapy. Major bleeding risk, and all cause mortality was comparable between both groups of patients.
Background
Atrial fibrillation is a common arrhythmia that increases the risk of stroke. However, treatment of such patients with oral anticoagulants when compared with aspirin is not well established with uncertain benefits.
Objective
We analyzed available study level data comparing Apixaban and Aspirin for efficacy and safety among atrial fibrillation patients.
Methods
We performed a systematic literature search on PubMed, EMBASE, and ClinicalTrials.gov for relevant randomized controlled trials (RCTs) from inspection until August 10th, 2024, without any language restrictions. Odds ratios (OR) and 95% confidence intervals (CI) were pooled using a random-effect model, and a p-value of <0.05 was considered statistically significant.
Results
A total of 3 RCTs with 14,224 patients were included (7,129 in apixaban and 7095 in the aspirin group) in the analysis. The mean age of the patients in apixaban and the aspirin groups was 72.4 and 72.8 years, respectively. Pooled analysis of primary and secondary endpoints showed that apixaban significantly reduced the risk of stroke or systemic embolism by 47% (OR, 0.53(95%CI: 0.38-0.75), P<0.001), stroke by 44% (OR, 0.56(95%CI: 0.44-0.70), P<0.001), and ischemic stroke by 51% (OR, 0.49(95%CI: 0.29-0.81), P=0.01) when compared with aspirin. However, the risk of major bleeding (OR, 1.03(95%CI: 0.69-1.53), P=0.88), myocardial infarction (OR, 0.97(95%CI: 0.76-1.23), P=0.78), and all-cause mortality (OR, 0.97(95%CI: 0.80-1.17), P=0.72) was comparable when compared with the aspirin group of patients.
Conclusion
In this comprehensive analysis of randomized controlled trials data, the use of apixaban was associated with reduction in stroke or systemic embolism, and ischemic stroke, when compared with aspirin therapy. Major bleeding risk, and all cause mortality was comparable between both groups of patients.
More abstracts on this topic:
Association of Ventricular Arrhythmias with Lamotrigine: An Observational Cohort Study
Kim Sodam, Welch Landon, De Los Santos Bertha, Radwanski Przemyslaw, Kim Kibum, Munger Mark
A Case Series of Papillary Fibroelastomas on the Coumadin ridgeAboukhatwa Omar, Akiki Elias, Kurmann Reto, Larson Kathryn, Keeney Michael, Bois Melanie, Klarich Kyle
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)