Final ID: WMP25
Predictors of Certified Stroke Center Presence in the Northeastern United States
Methods: Publicly available data from the U.S. Census Bureau and CDC Interactive Atlas of Heart Disease and Stroke were analyzed using a generalized linear model to examine the relationship between SC distribution and county demographics, stroke prevalence and mortality, and prevalence of stroke risk factors. Northeastern states were identified as Connecticut, Maine, Massachusetts, New Hampshire, New Jersey.
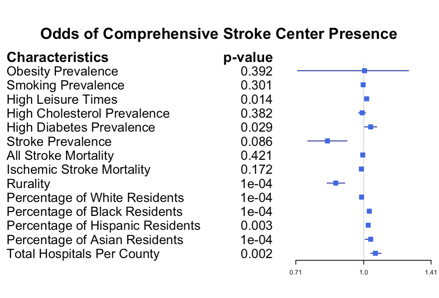
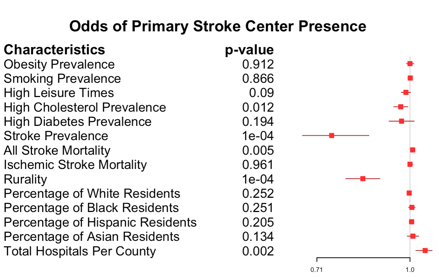
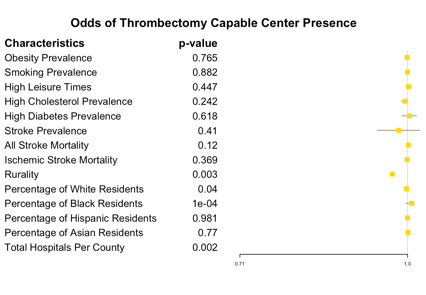
Results: Comprehensive (CSC) (adjusted odds ratio, 0.87 [95% CI, 0.83–0.91]; P<0.001), Primary (PSC) (adjusted odds ratio, 0.84 [95% CI, 0.79–0.89]; P<0.001), and Thrombectomy-Capable (TSC) (adjusted odds ratio, 0.97 [95% CI, 0.95–0.99]; P=0.003) center presence demonstrated a negative relationship with rurality. Lower overall SC density was observed in counties with high prevalence of hypercholesterolemia (adjusted odds ratio, 0.96 [95% CI, 0.93–0.99]; P=0.003). The absence of a CSC or PSC in a county was associated with a mean household income decrease of over $9,000 (P=0.005; P<0.001, respectively). Additionally, higher prevalence of stroke was associated with lower odds of PSC presence (adjusted odds ratio, 0.78 [95% CI, 0.67–0.90]; P<0.001).
Conclusion: This study reveals significant disparities in certified stroke center distribution in the northeastern U.S. While these centers reduce stroke mortality, their distribution does not uniformly reflect community needs. Of particular note was the negative association between stroke prevalence and the presence of PSCs, as PSCs often serve as the care access point for stroke patients in a hub-and-spoke system. These data point to a gap in access to specialized stroke care where it is most needed. Addressing the gap requires policymakers to consider both geographic and social factors, potentially expanding stroke centers in underserved regions to improve outcomes. Future research should focus on strategies to reduce these inequities and enhance access to stroke care.
More abstracts on this topic:
Cordero Christina, Llabre Maria, Romaker Emma, Kobayashi Marissa, Gianola Morgan, Gallo Linda, Isasi Carmen, Perreira Krista, Corsino Leonor, Zhou Laura
A Contemporary Machine Learning-Based Risk Stratification for Mortality and Hospitalization in Heart Failure with Preserved Ejection Fraction Using Multimodal Real-World DataFudim Marat, Weerts Jerremy, Patel Manesh, Balu Suresh, Hintze Bradley, Torres Francisco, Micsinai Balan Mariann, Rigolli Marzia, Kessler Paul, Touzot Maxime, Lund Lars, Van Empel Vanessa, Pradhan Aruna, Butler Javed, Zehnder Tobias, Sauty Benoit, Esposito Christian, Balazard Félix, Mayer Imke, Hallal Mohammad, Loiseau Nicolas
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.