Final ID: P2143
Adverse Pregnancy Outcomes – Planning for Fourth Trimester Interventions to Promote Equitable Long-Term Cardiovascular Health
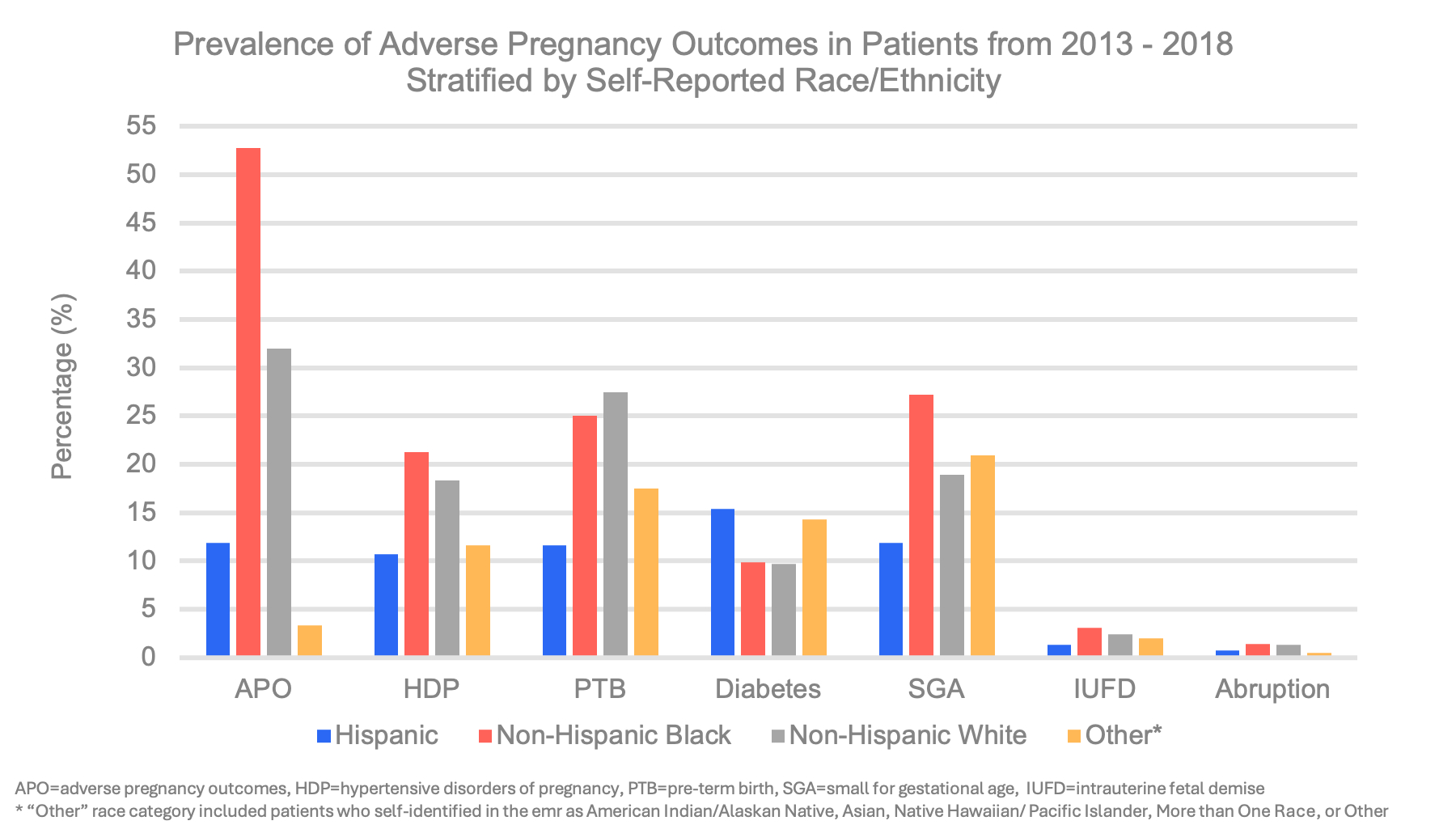
Abstract Body: Introduction: Adverse pregnancy outcomes (APOs) are significantly associated with future cardiovascular disease and cardiovascular mortality and disproportionately affect women from minority racial and ethnic groups. Maternal and perinatal morbidity in the Southeast US is among the highest in the country, and cardiovascular disease (CVD) is the #1 cause of death in pregnant and nonpregnant patients. Therefore, we sought to define the contemporary epidemiology of APOs among pregnant and postpartum individuals at a major tertiary center in the Southeast US to plan a fourth-trimester cardiovascular disease intervention. We assessed the hypothesis that there is racial and ethnic variation in the epidemiology of APOs.
Methods: We performed a retrospective study including pregnant/postpartum patients from a tertiary center between 2013 and 2018. The primary outcome was APO prevalence, defined as ≥1 of the following diagnoses during pregnancy or <6 weeks postpartum: hypertensive disorders of pregnancy (HDP), preterm birth (PTB), diabetes, placental abruption, intrauterine fetal demise (IUFD), and small for gestational age (SGA) neonate. Secondary outcomes included trends in APO prevalence, and prevalence of and adjusted relative risks (aRR) of APOs by self-reported race/ethnicity.
Results: Of 24,637 patients included in this study, all baseline characteristics significantly differed between groups. APOs occurred in 11,507 (47%) of pregnancies. Overall trends of HDP increased dramatically across the study period from 17% to 22% (p<0.001). APO prevalence in Non-Hispanic Black, Non-Hispanic White, and Hispanic individuals were significantly different at 53%, 32%, and 12% (p<0.001) (Figure). In adjusted analysis with Non-Hispanic White as a reference, Non-Hispanic Black individuals had an increased risk of APO aRR 1.03 (95% confidence interval (CI) 1.01-1.04), while Hispanic individuals had a reduced risk of APOs aRR 0.91 (95% CI 0.88-0.94). Hispanic individuals had an increased risk of diabetes aRR 1.73 (95% CI 1.51-1.94) while Non-Hispanic Black patients had an increased risk for IUFD aRR 1.33 (95% CI 1.05-1.60) and SGA aRR 1.32 (1.25-1.39).
Conclusion: Nearly half of the patients in the study period experienced an APO with marked racial/ethnic disparities. As APOs are associated with future CVD - the #1 cause of death - these findings underscore an urgent need for timely fourth-trimester interventions to promote equitable cardiovascular health.
Methods: We performed a retrospective study including pregnant/postpartum patients from a tertiary center between 2013 and 2018. The primary outcome was APO prevalence, defined as ≥1 of the following diagnoses during pregnancy or <6 weeks postpartum: hypertensive disorders of pregnancy (HDP), preterm birth (PTB), diabetes, placental abruption, intrauterine fetal demise (IUFD), and small for gestational age (SGA) neonate. Secondary outcomes included trends in APO prevalence, and prevalence of and adjusted relative risks (aRR) of APOs by self-reported race/ethnicity.
Results: Of 24,637 patients included in this study, all baseline characteristics significantly differed between groups. APOs occurred in 11,507 (47%) of pregnancies. Overall trends of HDP increased dramatically across the study period from 17% to 22% (p<0.001). APO prevalence in Non-Hispanic Black, Non-Hispanic White, and Hispanic individuals were significantly different at 53%, 32%, and 12% (p<0.001) (Figure). In adjusted analysis with Non-Hispanic White as a reference, Non-Hispanic Black individuals had an increased risk of APO aRR 1.03 (95% confidence interval (CI) 1.01-1.04), while Hispanic individuals had a reduced risk of APOs aRR 0.91 (95% CI 0.88-0.94). Hispanic individuals had an increased risk of diabetes aRR 1.73 (95% CI 1.51-1.94) while Non-Hispanic Black patients had an increased risk for IUFD aRR 1.33 (95% CI 1.05-1.60) and SGA aRR 1.32 (1.25-1.39).
Conclusion: Nearly half of the patients in the study period experienced an APO with marked racial/ethnic disparities. As APOs are associated with future CVD - the #1 cause of death - these findings underscore an urgent need for timely fourth-trimester interventions to promote equitable cardiovascular health.
More abstracts on this topic:
A Shocking Postpartum Course
Wozniak Phillip, Grodzinsky Anna
Advanced Lipid Status Parameters in Women With PreeclampsiaGojkovic Tamara, Saric Matutinovic Marija, Ivanisevic Jasmina, Vladimirov Sandra, Spasojevic Kalimanovska Vesna, Mikovic Zeljko, Stefanovic Aleksandra, Ardalic Daniela, Antonic Tamara, Banjac Gorica, Zeljkovic Aleksandra, Vekic Jelena, Miljkovic Trailovic Milica, Munjas Jelena, Jovicic Snezana