Final ID: TP139
Coordinating Stroke and Sleep Care with Field Staff and Champions: Difference-Makers in a Quality Improvement Program Addressing Sleep Apnea in Stroke Patients
Abstract Body: Background
The Addressing Sleep Apnea Post-Stroke/TIA (ASAP) clinical trial aimed to enhance OSA management at six VA medical centers through a hybrid implementation trial, requiring coordination across hospital medicine, sleep medicine, nursing, and neurology in both inpatient and outpatient settings. This analysis evaluated the trial’s efforts to standardize early OSA screening in stroke/TIA patients.
Methods
This mixed-methods evaluation used configurational comparative methods (CCMs) to identify key contextual factors for successful implementation, examining the joint effects of multiple factors. The stepped-wedge trial ran from May 2019 to January 2024 across three implementation waves. The primary outcome was the Group Organization (GO) score, which measured team cohesion in managing sleep apnea among cerebrovascular patients. Data sources included observational data, qualitative interviews, and administrative data across three periods (A, B, C), calibrated into dichotomous or multi-value categories for analysis.
Results
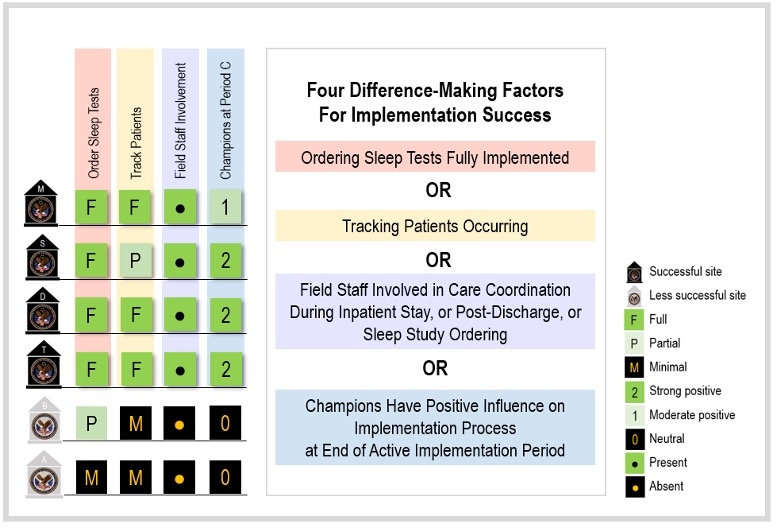
Four key difference-makers distinguished more successful sites (GO score ≥6) from others: routines for ordering inpatient OSA tests, patient care coordination during hospitalization, involvement of field staff, and strong local champions. The ability to order and complete sleep studies was crucial for timely OSA diagnosis. Field staff (e.g., respiratory technicians, polysomnographic technologists, research) played a critical role in coordinating care during inpatient stays and post-discharge. Key pathways to success included active field staff engagement and strong champion support, particularly in the final phase. Less successful sites faced barriers like geographic separation and staff shortages. The figure describes the values for each of these factors at the 4 more successful versus 2 less successful sites.
Conclusions
The study highlights the importance of flexibility in integrating new practices, particularly in stroke care requiring multi-specialty coordination. Findings provide a roadmap for healthcare systems implementing similar interventions, emphasizing leadership, coordinated care, and robust tracking for program success.
The Addressing Sleep Apnea Post-Stroke/TIA (ASAP) clinical trial aimed to enhance OSA management at six VA medical centers through a hybrid implementation trial, requiring coordination across hospital medicine, sleep medicine, nursing, and neurology in both inpatient and outpatient settings. This analysis evaluated the trial’s efforts to standardize early OSA screening in stroke/TIA patients.
Methods
This mixed-methods evaluation used configurational comparative methods (CCMs) to identify key contextual factors for successful implementation, examining the joint effects of multiple factors. The stepped-wedge trial ran from May 2019 to January 2024 across three implementation waves. The primary outcome was the Group Organization (GO) score, which measured team cohesion in managing sleep apnea among cerebrovascular patients. Data sources included observational data, qualitative interviews, and administrative data across three periods (A, B, C), calibrated into dichotomous or multi-value categories for analysis.
Results
Four key difference-makers distinguished more successful sites (GO score ≥6) from others: routines for ordering inpatient OSA tests, patient care coordination during hospitalization, involvement of field staff, and strong local champions. The ability to order and complete sleep studies was crucial for timely OSA diagnosis. Field staff (e.g., respiratory technicians, polysomnographic technologists, research) played a critical role in coordinating care during inpatient stays and post-discharge. Key pathways to success included active field staff engagement and strong champion support, particularly in the final phase. Less successful sites faced barriers like geographic separation and staff shortages. The figure describes the values for each of these factors at the 4 more successful versus 2 less successful sites.
Conclusions
The study highlights the importance of flexibility in integrating new practices, particularly in stroke care requiring multi-specialty coordination. Findings provide a roadmap for healthcare systems implementing similar interventions, emphasizing leadership, coordinated care, and robust tracking for program success.
More abstracts on this topic:
A Contactless and Automated Approach to the Acute Stroke Assessment
Saadat Moh, Titus Ryan, Verkuilen Haley, Fleming Phil, Sur Sanjib, Sen Souvik
Carotid body ablation reduces hypertension following long-term intermittent hypoxia by regulating brainstem glial cell activationIturriaga Rodrigo, Pereyra Katherine, Vicencio Sinay, Bernal Ignacio, Diaz-jara Esteban, Del Rio Rodrigo
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)