Final ID: WP220
Assessing the Therapeutic Time Window for Tranexamic Acid in Intracerebral Hemorrhage – A Systematic Review and Meta-analysis
Methods: We searched PubMed, Embase and Cochrane databases for randomized controlled trials (RCTs) published up to July 27, 2024 comparing TXA with placebo in ICH. We excluded trials that used TXA for longer than 3 days which causes delayed vasospasm, increasing the risk of cerebral ischemia. The primary outcomes were HE, 24-hour hemorrhagic volume change, 90-day mortality and poor functional outcome. We grouped the trials into 2 hours, 8 hours or 24 hours of TXA administration after hemorrhage onset. We pooled odds ratios (OR) and mean differences (MD) with 95% confidence intervals (CI) using Rstudio. Heterogeneity was examined with the I2 test.
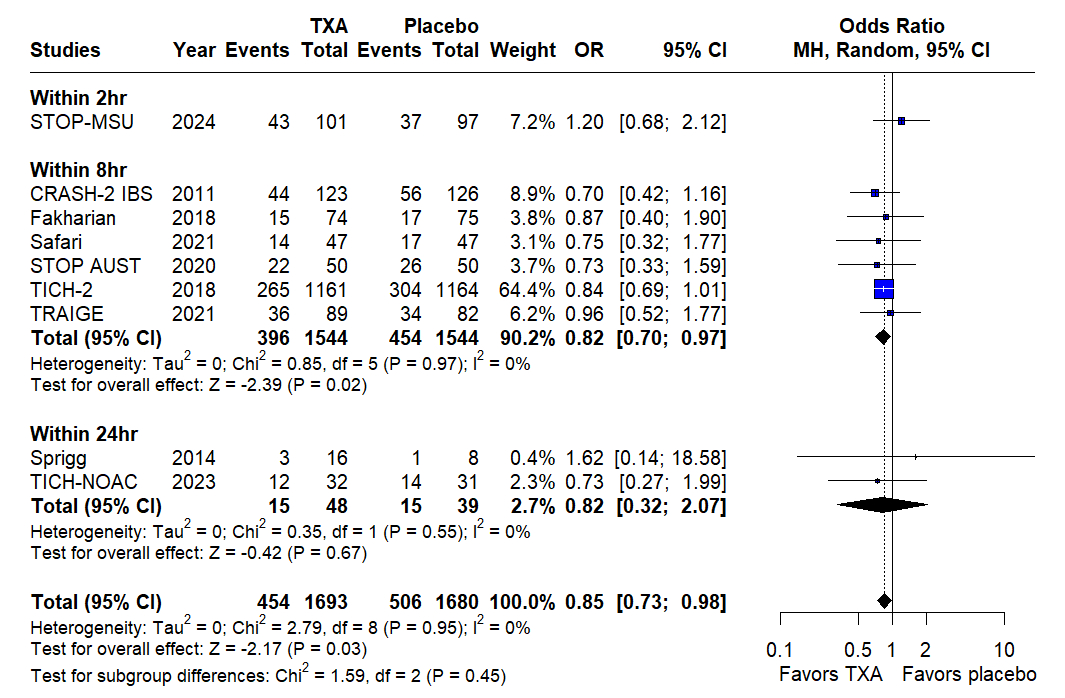
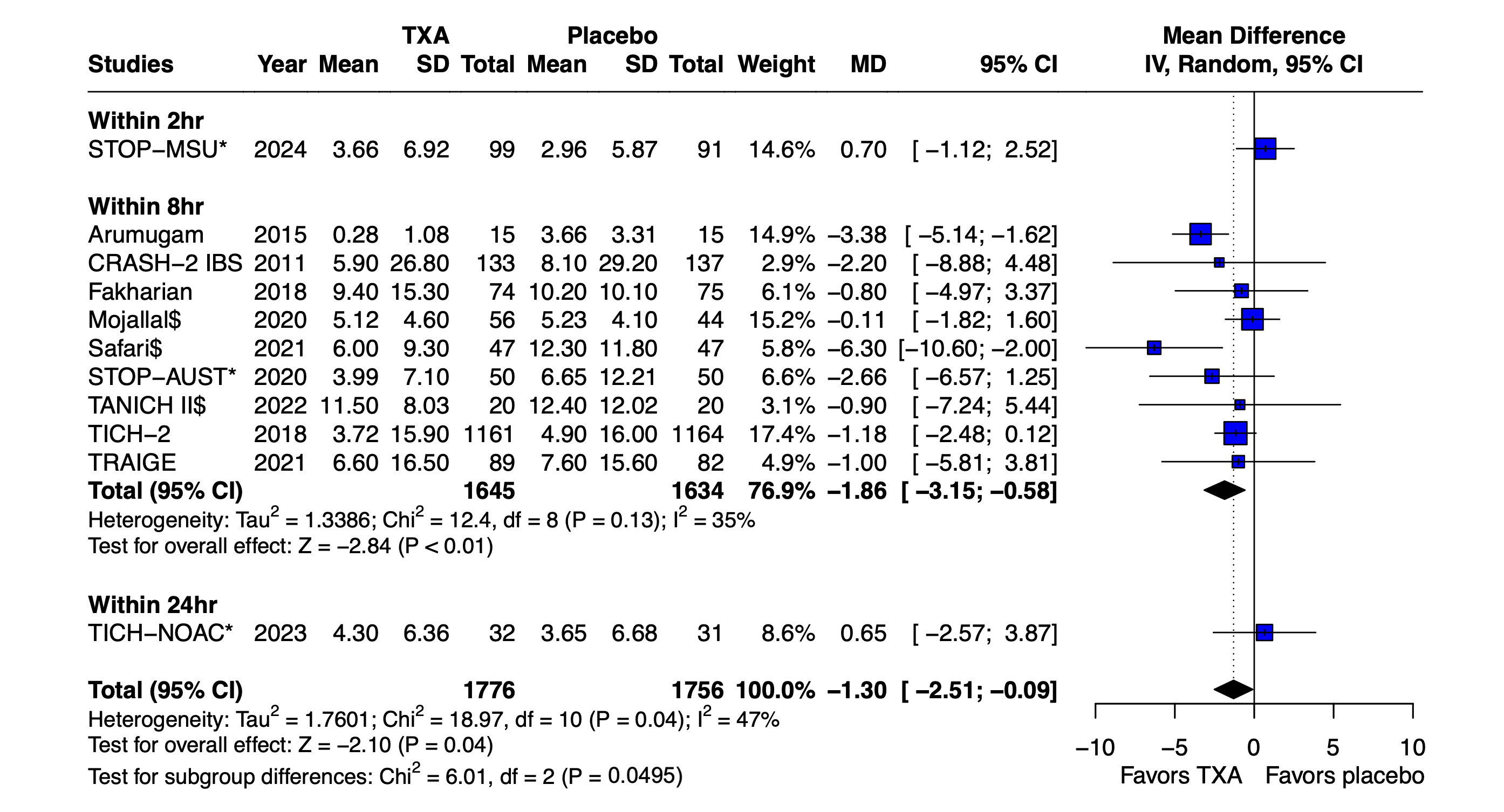
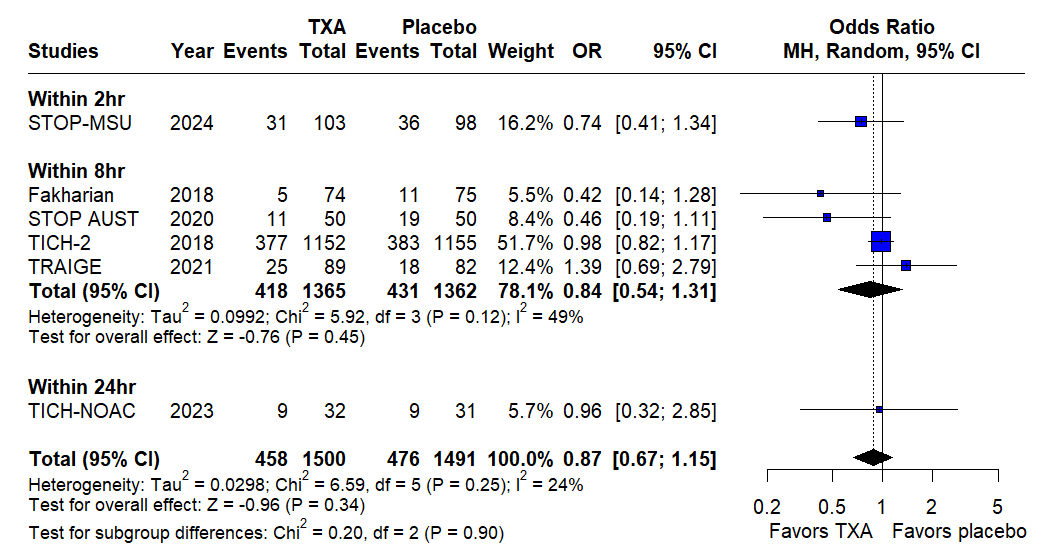
Results: We included 12 studies with 3,567 patients. Most of the studies used 1 g TXA in patients with Glasgow Coma Scale score ranging from 13-15. TXA reduced HE risk (OR 0.85; 95% CI 0.73 to 0.98; p= 0.03; I2= 0%). This reduction was observed in studies that administered TXA within 8 hours of ICH onset (OR 0.82; 95% CI 0.70 to 0.97; p= 0.02; I2= 0%). TXA slightly reduced 24-hour hemorrhagic volume (MD -1.30 mL; 95% CI -2.51; -0.09; p= 0.04; I2= 47%). This reduction was mainly seen in patients who were administered TXA within 8 hours of hemorrhage onset (MD -1.86 mL; 95% CI -3.15 to -0.58; p< 0.01; I2= 35%). There were no significant differences in poor functional outcome (OR 0.87; 95% CI 0.67 to 1.15; p= 0.34; I2= 24%), 90-day mortality (OR 1.00; 95% CI 0.84 to 1.19; p= 0.96; I2= 0%), major thromboembolic events (OR 1.22; 95% CI 0.82 to 1.82; p= 0.33; I2= 0%), neurosurgical intervention (OR 0.94; 95% CI 0.61-1.45; p= 0.78; I2= 0%) or length of hospital stay (MD -0.49 days; 95% CI -3.27 to 2.29; p= 0.73; I2= 0%).
Conclusion: TXA reduced the risk of HE and slightly reduced 24-hour hemorrhagic volume in patients with ICH within 8 hours. Larger RCTs stratifying administration timing are required to establish these findings.
More abstracts on this topic:
Ali Md Akkas, Vardaman, Donald, Bolding Chase, Tidwell Harrison, Tyrrell Daniel
A Phase 2a randomized controlled trial of once-daily versus twice-daily remote ischemic conditioning in vascular cognitive impairment (TRIC-VCI)Ganesh Aravind, Mccreary Cheryl, Sahlas Demetrios, Sharma Mukul, Swartz Richard, Smith Eric, Barber Philip, Black Sandra, Corbett Dale, Field Thalia, Frayne Richard, Hachinski Vladimir, Ismail Zahinoor, Mai Lauren
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.