Final ID: TMP2
Flow diversion treatments for unruptured intracranial aneurysms: real-world perioperative outcomes, hospital readmissions, and impact of comorbid anxiety and mood disorders
Methods: This was a retrospective analysis of the 2020-21 National Readmissions Database (NRD) in the United States. Patients who underwent elective FD placement were identified. Initial hospitalization outcomes were assessed. Patients who had an uncomplicated FD placement were followed for the calendar year for non-elective hospital readmissions. Risks of readmission for patients with and without baseline AMD were compared using Cox regression models adjusting for major confounders.
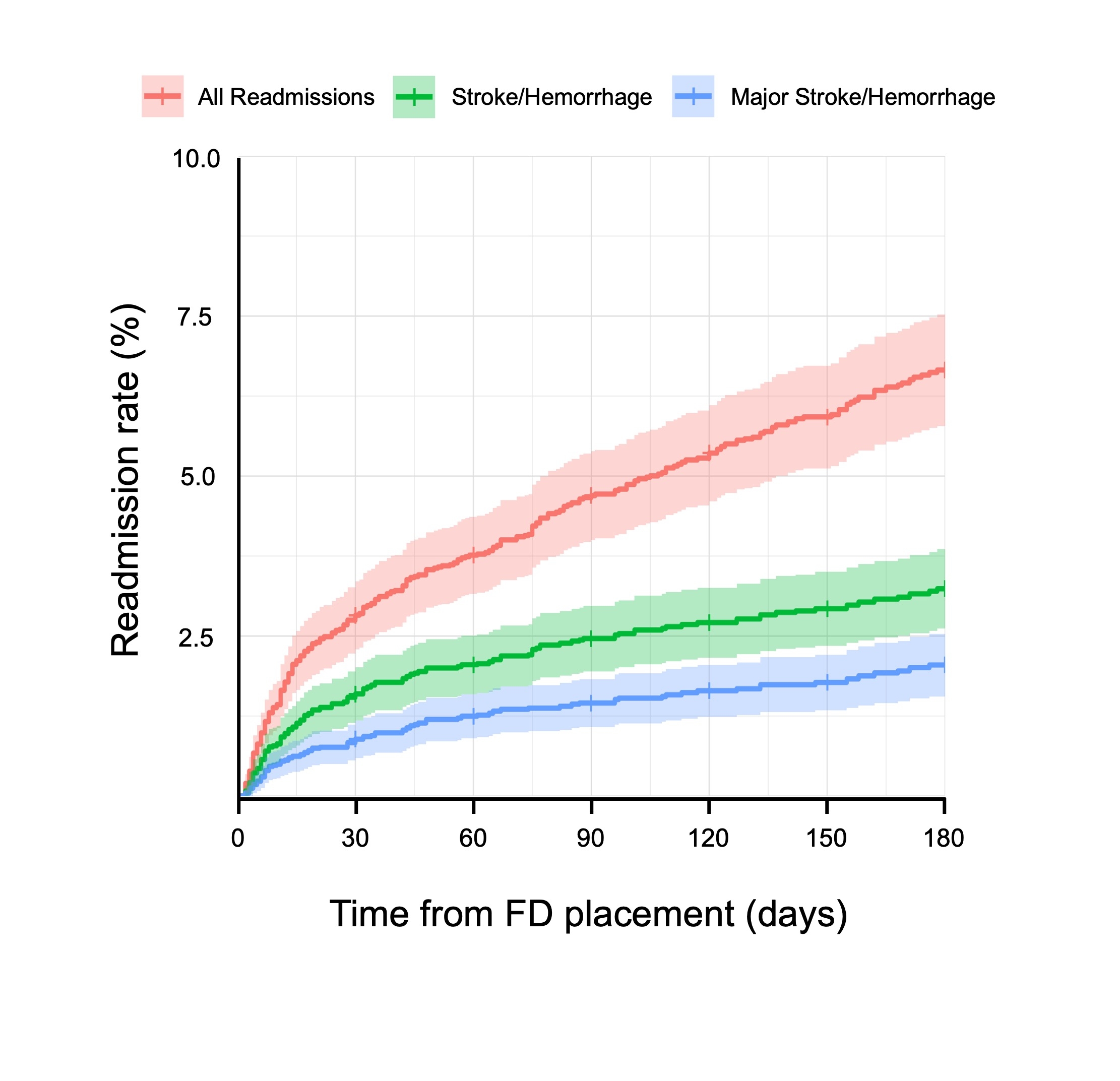
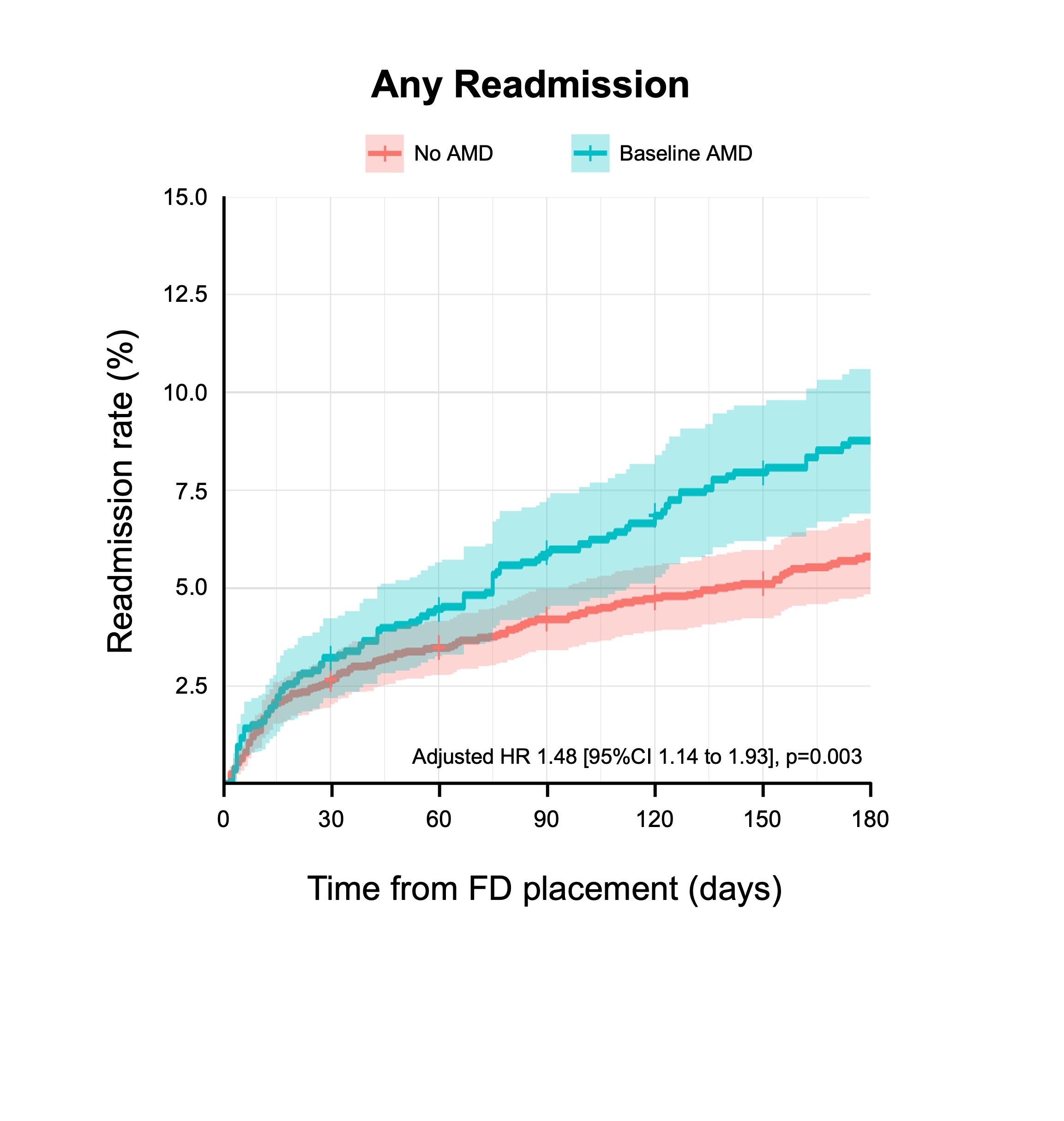
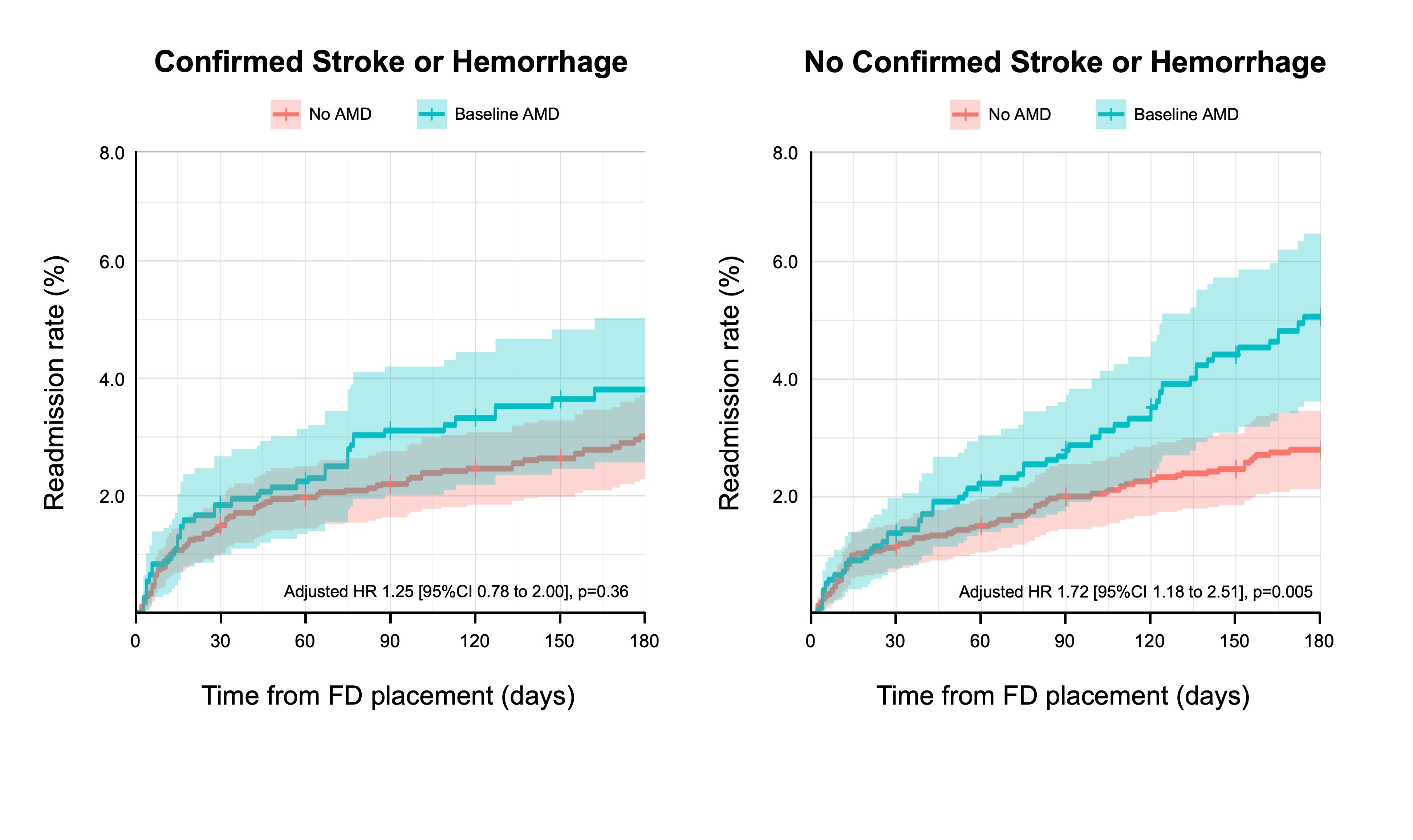
Results: 9,523 elective FD patients were identified, of whom 243 (2.6%) and 314 (3.3%) suffered perioperative stroke and intracranial hemorrhage (ICH), respectively, and 2,800 (29.4%) had baseline AMD. Six-month readmission rate for any reason, stroke or hemorrhage, and major stroke or hemorrhage (that led to patient morbidity or mortality) were 6.9%, 3.9%, and 1.8%, respectively (Figure 1). Patients with baseline AMD had a significantly higher risk of overall hospital readmissions than those without (adjusted hazards ratio 1.48 [95%CI 1.14 to 1.93], p=0.003; Figure 2). Further analyses revealed that patients with baseline AMD did not have a higher risk of any stroke or hemorrhage confirmed during readmissions (HR 1.25 [95%CI 0.78-2.00], p=0.36; Figure 3), but they did have a significantly higher risk of readmissions without confirmed stroke or hemorrhage (HR 1.72 [95%CI 1.18 to 2.51], p=0.005; Figure 3). Among readmitted AMD patients without confirmed stroke or hemorrhage, 15.4% suffered short-term morbidity, which incurred a median cost of $11,725 USD per patient.
Conclusions: In routine United States clinical practice, the perioperative risks of stroke and ICH for FD patients were 2.6% and 3.3% respectively, and the risk major stroke or hemorrhage within 6 months after hospital discharge was 1.8%. Baseline AMD was associated with a significantly increased risk of hospital readmissions without confirmed stroke or hemorrhage, highlighting the need for a better understanding of how comorbid AMD may impact patient outcomes following FD.
More abstracts on this topic:
Xu Qinzi, Rochon Elizabeth, Bocian Kaitlin, Huang Xue, Poropatich Ronald, Gladwin Mark, Tejero Jesus, Rose Jason, Rodriguez Deborah, Hwang Hyon, Turner Bryan, Hunt Thomas, Dent Matthew, Demartino Anthony, Abdelghany Youmna, Chen Xiukai
Association of Stroke Severity with Post-Stroke Depression and Household SizeCahuiche Ana, Petway Ana, Enochs Carolyn, Couture Lucy, Delevati Colpo Gabriela, Mccullough Louise
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.