Final ID: WP92
Prehospital FAST-ED Score Component Agreement to Corresponding In-hospital NIHSS Component Scores
Abstract Body: Background
Emergency Medical Services (EMS) can shorten the time to endovascular treatment by transporting Large Vessel Occlusion (LVO) Acute Ischemic Stroke (AIS) patients directly to thrombectomy centers. The most common prehospital strategy for identifying LVO AIS is performing an LVO screen. In 2019, our county EMS system implemented the Field Assessment Stroke Triage for Emergency Destination (FAST-ED) score as its LVO screen. Our objective was to assess the agreement of the FAST-ED score components performed by the paramedic in the field with the corresponding components of the National Institute of Health Stroke Scale (NIHSS) performed by the hospital neurologist for patients discharged with an ischemic stroke diagnosis.
Methods
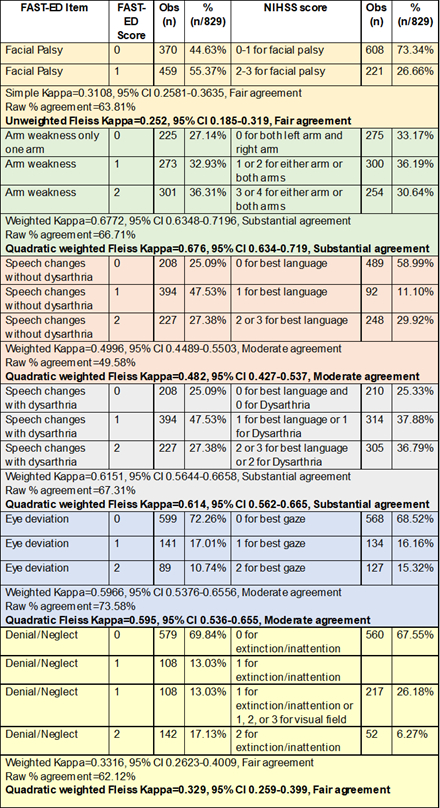
From a prospectively maintained database of consecutive patients ≥ 18 years old transported to one of four hospitals by our county EMS agency with a FAST-ED score documented, we conducted a retrospective study of patients diagnosed with AIS for whom the Code Stroke protocol was activated. Corresponding component score agreement was measured using unweighted Fleiss Kappa for the dichotomized measure of facial palsy and quadratic Fleiss’ Kappa for the other ordinal measures. Since ambiguity exists regarding the inclusion of dysarthria without aphasia in the FAST-ED speech changes score, agreement for that component score was compared to dysarthria and/or aphasia.
Results
From September 2019 to March 2024, we identified 829 patients meeting our inclusion criteria. The median time interval from hospital arrival to CT performance as an index of NIHSS performance time was 10 minutes (IQR 8-15). The items with substantial agreement were arm weakness (Kappa=0.676, 95% CI 0.634-0.719) and speech changes defined as dysarthria and/or aphasia (Kappa=0.614, 95% CI 0.562-0.665). Moderate agreement was found for eye deviation (Kappa=0.595, 95% CI 0.536-0.655) and speech changes not including dysarthria (Kappa=0.482, 95% CI 0.427-0.537). There was only fair agreement for facial palsy (Kappa=0.252, 95% CI 0.185-0.319) and denial/neglect (Kappa=0.329, 95% CI 0.259-0.399)
Conclusions
EMS providers may benefit from targeted education in assessing denial/neglect and facial palsy when they are components of LVO screens. The FAST-ED score would benefit from increased clarity regarding the inclusion of isolated dysarthria as scoring positive for a speech change.
Emergency Medical Services (EMS) can shorten the time to endovascular treatment by transporting Large Vessel Occlusion (LVO) Acute Ischemic Stroke (AIS) patients directly to thrombectomy centers. The most common prehospital strategy for identifying LVO AIS is performing an LVO screen. In 2019, our county EMS system implemented the Field Assessment Stroke Triage for Emergency Destination (FAST-ED) score as its LVO screen. Our objective was to assess the agreement of the FAST-ED score components performed by the paramedic in the field with the corresponding components of the National Institute of Health Stroke Scale (NIHSS) performed by the hospital neurologist for patients discharged with an ischemic stroke diagnosis.
Methods
From a prospectively maintained database of consecutive patients ≥ 18 years old transported to one of four hospitals by our county EMS agency with a FAST-ED score documented, we conducted a retrospective study of patients diagnosed with AIS for whom the Code Stroke protocol was activated. Corresponding component score agreement was measured using unweighted Fleiss Kappa for the dichotomized measure of facial palsy and quadratic Fleiss’ Kappa for the other ordinal measures. Since ambiguity exists regarding the inclusion of dysarthria without aphasia in the FAST-ED speech changes score, agreement for that component score was compared to dysarthria and/or aphasia.
Results
From September 2019 to March 2024, we identified 829 patients meeting our inclusion criteria. The median time interval from hospital arrival to CT performance as an index of NIHSS performance time was 10 minutes (IQR 8-15). The items with substantial agreement were arm weakness (Kappa=0.676, 95% CI 0.634-0.719) and speech changes defined as dysarthria and/or aphasia (Kappa=0.614, 95% CI 0.562-0.665). Moderate agreement was found for eye deviation (Kappa=0.595, 95% CI 0.536-0.655) and speech changes not including dysarthria (Kappa=0.482, 95% CI 0.427-0.537). There was only fair agreement for facial palsy (Kappa=0.252, 95% CI 0.185-0.319) and denial/neglect (Kappa=0.329, 95% CI 0.259-0.399)
Conclusions
EMS providers may benefit from targeted education in assessing denial/neglect and facial palsy when they are components of LVO screens. The FAST-ED score would benefit from increased clarity regarding the inclusion of isolated dysarthria as scoring positive for a speech change.
More abstracts on this topic:
Acoustic Biomarkers Harvested from 911 Calls Differ among Patients with Cardiac and Non-Cardiac Chest Pain
Mazhar Harris, Zegre-hemsey Jessica, Lee Kyungbok, Tian Baotong, Heydari Mojtaba, Cushman Jeremy, Duan Zhiyao, Dzikowicz Dillon
Association between delta ETCO2 and Return of Spontaneous Circulation in a National US CohortGrabman Bartholomew, Fisher Benjamin, Mann N. Clay, Braude Darren, Huebinger Ryan
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)