Final ID: DP17
Higher Pre-Admission Blood Pressure Is Associated with Lower Initial Infarct Volume after Acute Large Vessel Occlusions
Abstract Body: Introduction
Following a large vessel occlusion acute ischemic stroke (LVO-AIS), cerebral autoregulation is notably compromised, making cerebral blood flow maintenance and optimal blood pressure (BP) crucial to preserving the penumbral tissue until reperfusion. While intraprocedural BP drops and high post mechanical thrombectomy (MT) BP are associated with unfavorable outcomes, data on pre-admission BP's impact on infarct growth is markedly scarce.
Methods
This retrospective cohort study from two centers included anterior circulation LVO-AIS patients treated with MT from Jan-2018 to Dec-2021. Admission CTP parameters were: Initial infarct volume (rCBF<30%), hypoperfused tissue (Tmax>4s,6s,8s,10s). Hypoperfusion intensity ratio (HIR, Tmax 10s/6s) served as a collateral status surrogate. Infarct growth rate (IGR) was defined as rCBF<30%/stroke onset-to-CTP time. BP, measured with non-invasive cuffs, was obtained from Emergency Medical Services reports. For each patient, mean SBP (mSBP), mean MAP (mMAP) and BP drops (difference between highest and lowest MAP) were calculated. We used multivariable regression to evaluate associations between hemodynamic and neuroimaging parameters.
Results
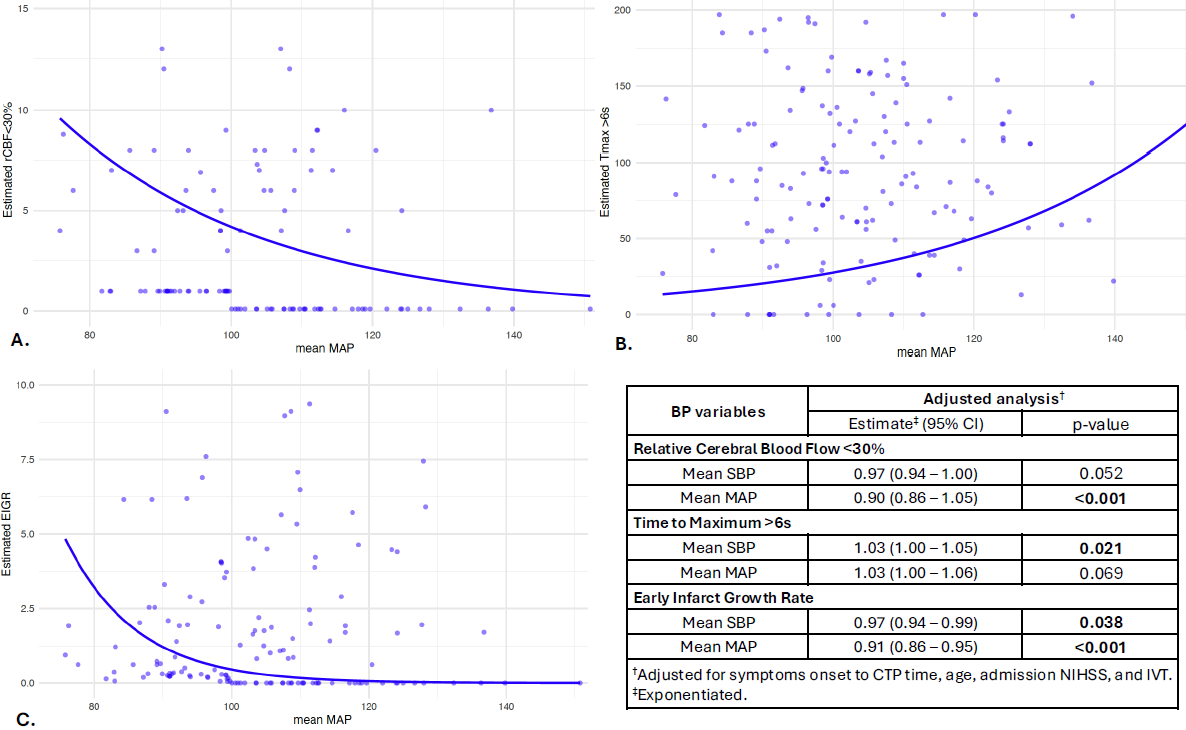
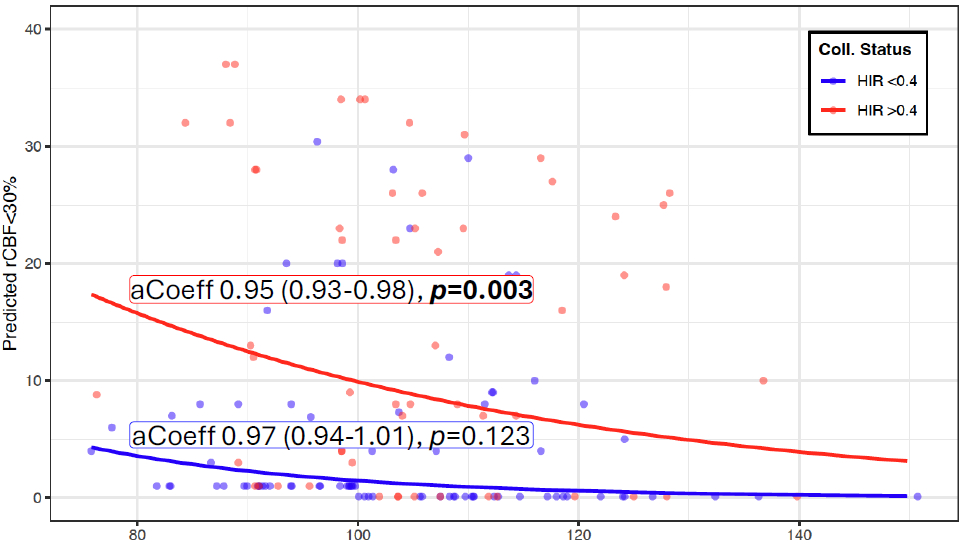
171 patients were included in the study. Median age was 71 yrs [IQR 64–81], and 48.5% were women. 117 patients (92.9%) had baseline mRS 0-2, median NIHSS and ASPECTS were 15 [10–20] and 8 [7-9]. Median mSBP was 145 mmHg [134–162], median mMAP 104 [94–112] and median dMAP 17 mmHg [12-30]. For each unit increase in mMAP, the rCBF<30% decreased by 10% (adjusted coefficient 0.90, p<0.001), and the IGR decreased in 9% (aCoeff. 0.91, p<0.001) after adjusting for symptoms onset to CTP time, age, admission NIHSS and IVT. For each unit increase in mean SBP, Tmax >6s increased by 3% (aCoeff. 1.03, p=0.021), and IGR decreased in 3% (aCoeff. 0.97, p=0.038) (Figure 1). Importantly, the association between mMAP and lower rCBF<30% was higher in patients with good collateral status stratified by HIR 0.4 (Figure 2).
Conclusion
Higher pre-admission mMAP is linked to reduced initial infarct volume, and both mMAP and mSBP are associated with slower early IGR. These findings were consistent in patients with favorable collateral status, as opposed to patients with poor collaterals. These insights underscore the complex role of BP management in LVO-AIS and the need for further prospective studies on BP interventions targeting high BP preservation, while considering individual hemodynamics.
Following a large vessel occlusion acute ischemic stroke (LVO-AIS), cerebral autoregulation is notably compromised, making cerebral blood flow maintenance and optimal blood pressure (BP) crucial to preserving the penumbral tissue until reperfusion. While intraprocedural BP drops and high post mechanical thrombectomy (MT) BP are associated with unfavorable outcomes, data on pre-admission BP's impact on infarct growth is markedly scarce.
Methods
This retrospective cohort study from two centers included anterior circulation LVO-AIS patients treated with MT from Jan-2018 to Dec-2021. Admission CTP parameters were: Initial infarct volume (rCBF<30%), hypoperfused tissue (Tmax>4s,6s,8s,10s). Hypoperfusion intensity ratio (HIR, Tmax 10s/6s) served as a collateral status surrogate. Infarct growth rate (IGR) was defined as rCBF<30%/stroke onset-to-CTP time. BP, measured with non-invasive cuffs, was obtained from Emergency Medical Services reports. For each patient, mean SBP (mSBP), mean MAP (mMAP) and BP drops (difference between highest and lowest MAP) were calculated. We used multivariable regression to evaluate associations between hemodynamic and neuroimaging parameters.
Results
171 patients were included in the study. Median age was 71 yrs [IQR 64–81], and 48.5% were women. 117 patients (92.9%) had baseline mRS 0-2, median NIHSS and ASPECTS were 15 [10–20] and 8 [7-9]. Median mSBP was 145 mmHg [134–162], median mMAP 104 [94–112] and median dMAP 17 mmHg [12-30]. For each unit increase in mMAP, the rCBF<30% decreased by 10% (adjusted coefficient 0.90, p<0.001), and the IGR decreased in 9% (aCoeff. 0.91, p<0.001) after adjusting for symptoms onset to CTP time, age, admission NIHSS and IVT. For each unit increase in mean SBP, Tmax >6s increased by 3% (aCoeff. 1.03, p=0.021), and IGR decreased in 3% (aCoeff. 0.97, p=0.038) (Figure 1). Importantly, the association between mMAP and lower rCBF<30% was higher in patients with good collateral status stratified by HIR 0.4 (Figure 2).
Conclusion
Higher pre-admission mMAP is linked to reduced initial infarct volume, and both mMAP and mSBP are associated with slower early IGR. These findings were consistent in patients with favorable collateral status, as opposed to patients with poor collaterals. These insights underscore the complex role of BP management in LVO-AIS and the need for further prospective studies on BP interventions targeting high BP preservation, while considering individual hemodynamics.
More abstracts on this topic:
A small peptide eCIRP inhibitor attenuates neuroinflammation and reduces brain injury in ischemic stroke.
Lapin Dmitriy, Sharma Archna, Wang Ping
Bilateral Vertebral Artery Stenosis and Severe Aortic Valve Stenosis Trigger Functional Hypotension With Neurologic Collapse and SyncopeKilic Abdullah, Waheed Tallha, Ghani Samrah, Soliman Isaac, Armstrong David
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)