Final ID: WP216
Initial Imaging Markers Correlate with Increased Intracavitary Bleeding and Decreased Evacuation Rate Following Minimally Invasive ICH Evacuation
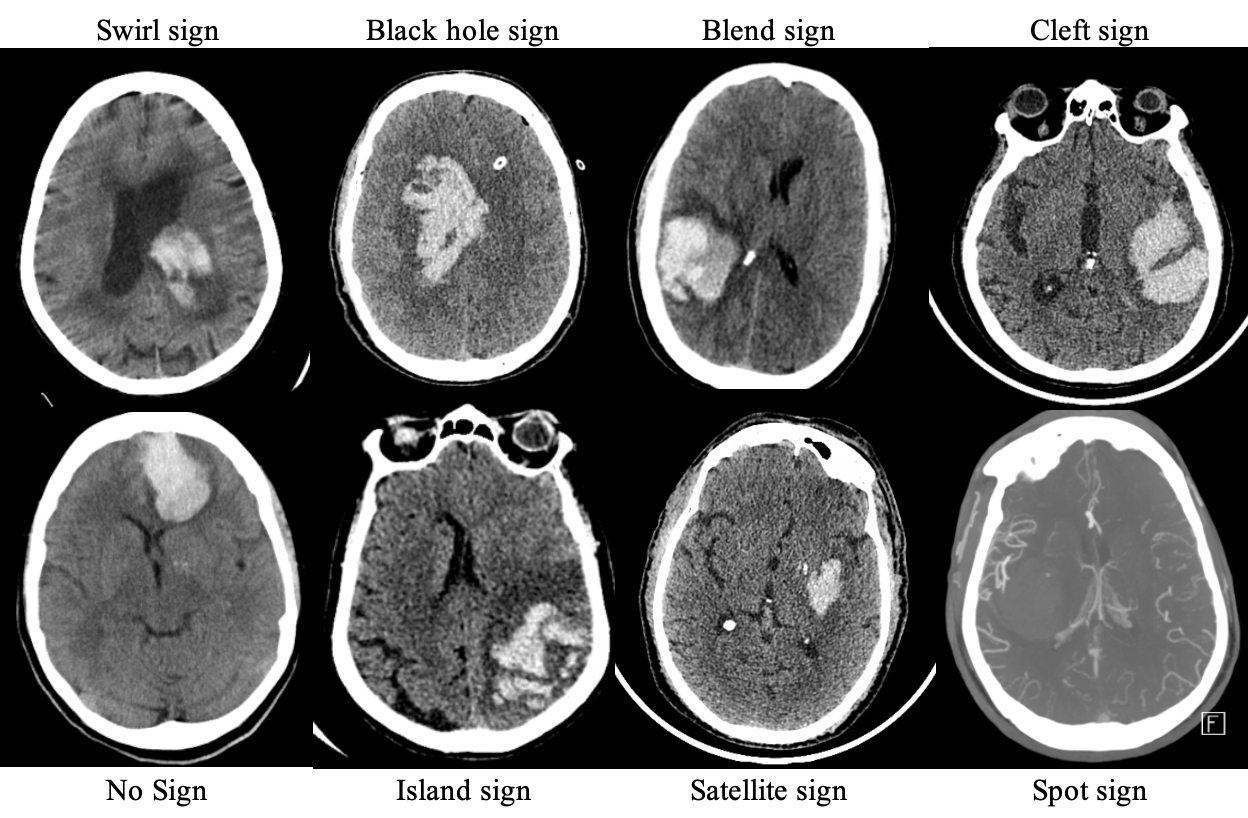
Methods: This study included all patients presenting with ICH who underwent MIS ICH evacuation from 2016 to 2021. The presence of spot sign, swirl sign, blend sign, black hole sign, satellite sign, island sign, and cleft was identified on pre-operative CT imaging. Univariate and multivariate analyses were performed between CT markers and variables of operative outcome with R v 4.3.1.
Results: 221 patients met the inclusion criteria. Swirl sign was identified in 127 patients (57%), spot sign in 30 (14%), black hole sign in 60 (27%), island sign in 10 (5%), satellite sign in 63 (29%), blend sign in 32 (14%), and cleft in 59 (27%). On univariate analysis, presence of any hematoma characteristic was correlated with increased intracavitary bleeding score (2.61±1.35 vs. 2.00±1.94, p = 0.027). Spot sign was correlated with increased rate of surgical rebleed (3.7% vs 2.4%, p = 0.021). Satellite sign was correlated with increased rate of surgical rebleed (6.7% vs. 0.7%, p = 0.021) and marginally significant increased residual volume (12±17 mL vs. 8±11 mL, p = 0.066). Presence of a cleft within hematoma was correlated with decreased evacuation rate (0.76±0.21 vs. 0.85±0.2, p = 0.005), increased intracavitary bleeding score (3.03±1.44 vs. 2.39±1.22, p = 0.019), increased residual volume (14±13 vs. 7±12, p = 0.001), increased presence of amyloid (31% vs 17%, p = 0.034). Multivariate linear regression analysis of presence of cleft controlling for pre-operative hematoma volume predicted increased bleeding score by 0.56 (p = 0.026), and on separate analysis predicted decreased evacuation rate by 9% (p = 0.005). Multivariate ordinal regression analysis of presence of cleft controlling for pre-operative hematoma volume predicted increased probability of increased bleeding by 117% (OR 2.17, CI: 1.09 - 4.39, p = 0.029).
Conclusions: Preoperative hematoma heterogeneity, specifically presence of cleft, is associated with increased intracavitary bleeding, decreased evacuation rate and increased residual volume following MIS ICH evacuation. Understanding the impact of hematoma characteristics is integral for patient selection in MIS ICH evacuation and postoperative care planning.
More abstracts on this topic:
Nariman Nina, Boren Seth, Hasan Khader, Suchting Robert, De Dios Constanza, Sitton Clark, Aronowski Jaroslaw, Savitz Sean, Haque Muhammad
Association of Biomarkers with risk of Hematoma Expansion and Arterial Thromboembolic Events in Acute Factor Xa Inhibitor-Associated Intracerebral Hemorrhage: The ANNEXa-I Biomarker SubstudyShoamanesh Ashkan, Verhamme Peter, Eikelboom John, Sharma Mukul, Xu Lizhen, Bamberg Krister, Beyer-westendorf Jan, Falkenberg Cecilia, Ladenvall Per, Narayan Rohit, Penland Robert
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.