Final ID: WP144
Impact of the Veterans Health Administration National Telestroke Program's Inpatient Subacute Telestroke Consult Service Implementation on Interhospital Transfers
Telestroke improves access to vascular neurology expertise and aids in decision-making for acute ischemic stroke (AIS). Prior studies from the Veterans Health Administration (VHA) demonstrated that the implementation of an acute national telestroke program (NTSP) led to reduction in interhospital transfer rates. Few studies have examined subacute inpatient telestroke services, focusing on inpatient stroke workup and management. We sought to determine the impact of a novel subacute telestroke program on emergency department (ED) transfer rates at participating hospitals.
Methods
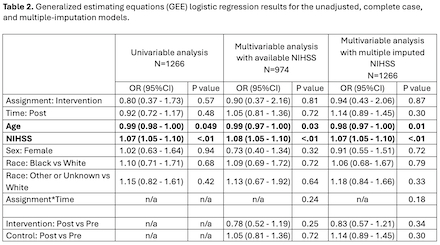
This was a retrospective cohort study of patients with ED diagnosis of AIS from 10/2021-6/2024. For intervention sites, the period prior to subacute consult “go-live” date was considered the pre-implementation period. Control sites (NTSP acute telestroke sites that had limited ED/inpatient neurology coverage and had expressed interest in the program) were considered pre-implementation prior to 5/22/2023 (the date when approximately half of intervention sites had initiated the subacute program). Logistic regression with a generalized estimating equation approach to handle clustering within facility was used to evaluate the association between implementation time-period (post/pre) and odds of ED transfer (yes/no) in intervention and control sites, adjusting for age, NIHSS, sex, race, and an intervention by time-period interaction term. Given NIHSS missingness of 23%, multiple-imputation using predictive mean matching was performed.
Results
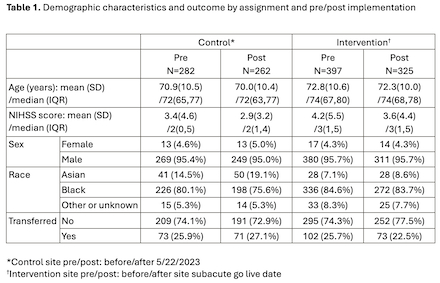
1266 patients met eligibility criteria (N=544 patients from 11 control sites and N=722 patients from 11 intervention sites). The ED transfer rate was lower within intervention sites post-implementation (pre: 25.7% to post: 22.5%) and higher in control sites (pre: 25.9% to post: 27.1% ; Table 1). These comparisons were statistically nonsignificant in the multivariable analysis for both complete case and multiple-imputed models where younger age and increased NIHSS were associated with increased odds of transfer (Table 2).
Discussion
There was a numerical reduction in interhospital transfers for AIS among intervention sites after implementation of a subacute telestroke consultation service, but the results were statistically nonsignificant in adjusted models. Future analyses should evaluate whether receipt of a subacute telestroke encounter at the patient-level is associated with reduced interhospital transfer for stroke.
More abstracts on this topic:
Velasco Claudia Mae, Baksh Gladys, Reesor Heather, Haydo Michele, Ali Omaima
Evaluating the Implementation of Brainomix 360 AI Stroke Software in a Robust Academic Hub-and-Spoke Telestroke NetworkSmith Brett, Woodhead Zoe, Harston George, English Stephen, Wolfe Jackson, Karam Alvina, Demaerschalk Bart, Hrdlicka Courtney, Nasr Deena, Chukwudelunzu Felix, Nord Charisse, Pahl Emily
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.