Final ID: WMP78
Dynamic Predictive Model for Gastrostomy Tube Placement after Acute Ischemic Stroke: A Single Center Study
Methods: Pooled clinical data of consecutive adult stroke patients from a single center from April - December 2023 were retrospectively collected. Patient baseline characteristics, demographics, imaging findings, and clinical assessments were assessed in regards to gastrostomy tube placement. Using a Lasso procedure, features with an independent association with gastrostomy tubes were found. An XGBoost model was used to predict placement of a gastrostomy tube to derive a final scoring model based on feature importance using Shapley values.
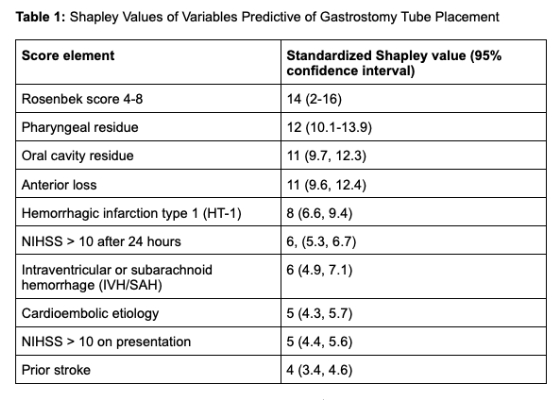
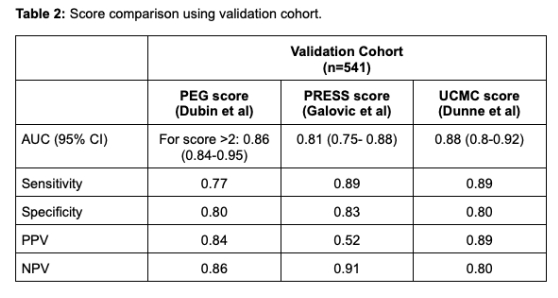
Results: Of the 635 patients screened, 74 (10.4%) underwent gastrostomy tube placement. Demographic and clinical gastrostomy placement predictors were identified and included Rosenbek scores 4-8, pharyngeal residue rating, oral cavity residue rating, Anterior loss on dysphagia assessment, hemorrhagic infarction type 1 (HT-1), National Institutes of Health Stroke Scale (NIHSS) > 10 after 24 hours, intraventricular or subarachnoid hemorrhage (IVH/SAH), cardioembolic etiology, NIHSS > 10 on presentation, and prior stroke. The comprehensive model unbiased estimated out-of-sample performance, using a 10-fold cross-validated area under the curve (AUC), was 0.81 [0.77-0.85]. The simplified scoring model performed similarly to the comprehensive model, although slightly higher than expected given a lack of an independent out-of-sample testing set due to data availability, with an AUC of 0.88 [0.80, 0.92]. This outperformed the previously published PEG score (0.86 [0.84-0.95]) and PRESS score (0.81 [0.75- 0.88]). However, a completely out-of-sample evaluation of the final scoring model remains necessary.
Conclusions: This scoring system provides clinically relevant predictive value to identify acute ischemic stroke patients who will ultimately require gastrostomy tubes as opposed to those who experience transient dysphagia and premature gastrostomy tube placement can be avoided. Future studies will be required to determine if this scoring system can result in reductions in hospital stays and other clinical outcomes.
More abstracts on this topic:
Suzuki Kentaro, Kutsuna Akihito, Katano Takehiro, Otsuka Toshiaki, Kimura Kazumi, Onodera Hidetaka, Sugiyama Rie, Okubo Seiji, Kimura Naoto, Shogo Kaku, Seki Rieko, Fujita Satoshi, Nomura Koichi
DOES PHARYNGEAL ELECTRICAL STIMULATION IMPROVE SWALLOWING IN ACUTE STROKE DYSPHAGIA? THE PHEAST TRIAL.Bath Philip, Smith Craig, Sprigg Nikola, Woodhouse Lisa, England Tim, Everton Lisa, Hamdy Shaheen, Hamilton Tiffany, James Marilyn, Montgomery Alan, Skinner Cameron
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.