Final ID: 104
Theoretical effect of PCSK9 inhibitor use in the SAMMPRIS trial: A secondary analysis of LDL lowering
Abstract Body: Introduction: The risk of recurrent atherosclerotic vascular events in patients with stroke due to intracranial atherosclerotic disease (ICAD) is high, and can be reduced with aggressive medical management. Novel lipid-lowering therapies such as proprotein convertase subtilisin/kexin type 9 inhibitors (PCSK9i) can dramatically lower low-density lipoprotein (LDL) and lipoprotein(a) levels, but are not presently indicated for stroke due to ICAD.
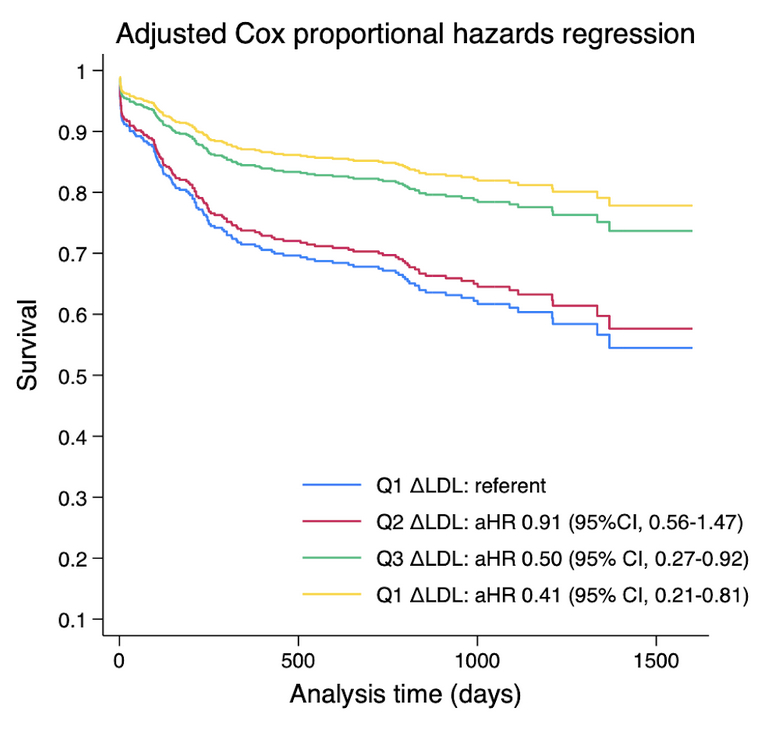
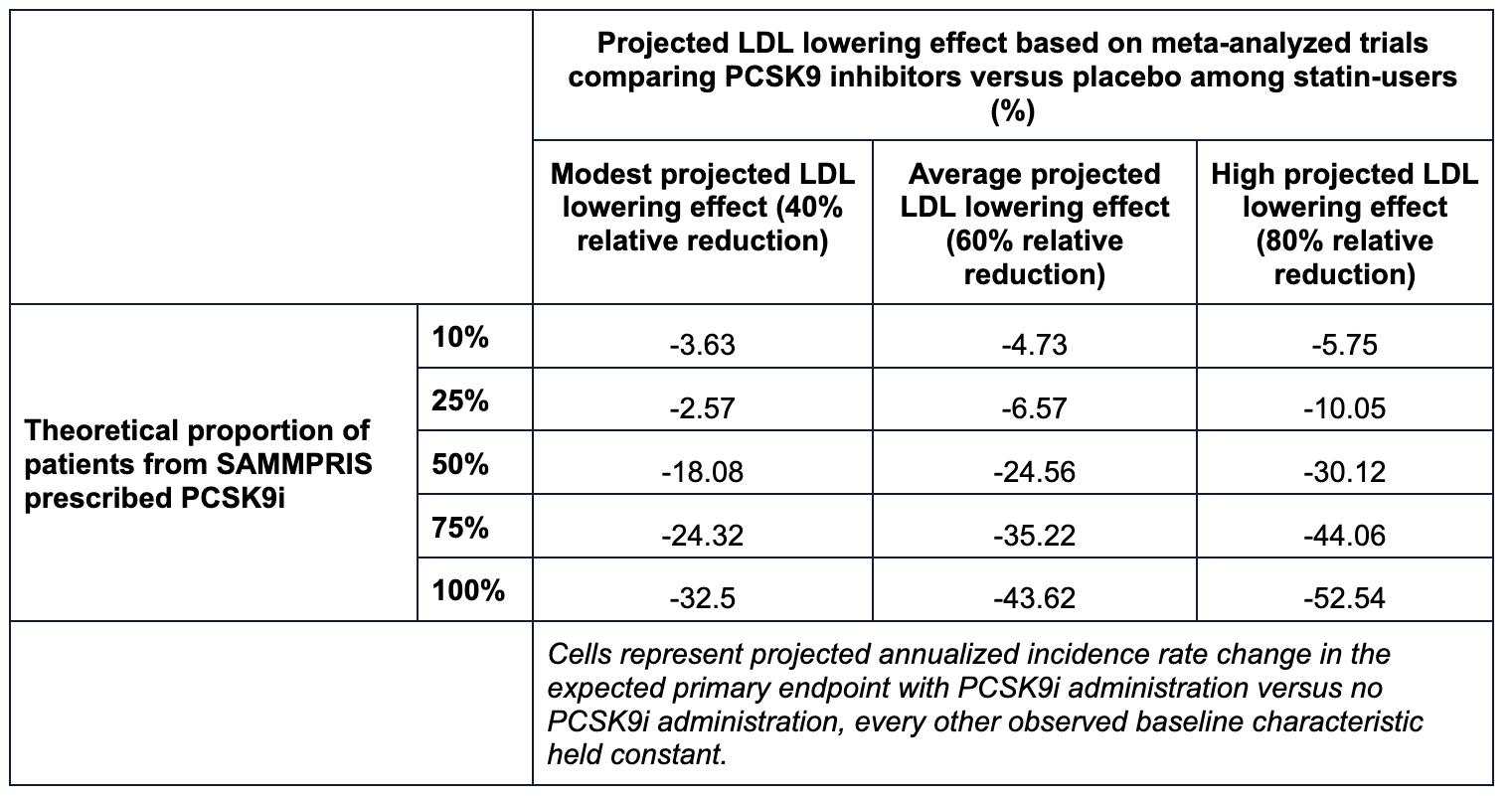
Methods: We conducted a secondary analysis of the SAMMPRIS clinical trial to estimate the association between changes in LDL and a composite outcome of first ischemic stroke, myocardial infarction, or death. Estimates were assessed using an adjusted Cox proportional hazards model accounting for age, sex, race, Hispanic ethnicity, baseline LDL level, vascular comorbidities, and use of intracranial stenting. We applied relative LDL reduction estimates from meta-analyzed trial data evaluating the effect of PCSK9i versus placebo among statin users with atherosclerotic vascular disease to project adjusted incidence rate differences of the primary outcome observed in SAMMPRIS with an equivalent LDL reduction. Semiparametric Cox proportional hazards models estimated the annualized relative risk of primary events if PCSK9i were used with aggressive risk factor modification for stroke due to ICAD.
Results: Of the 451 patients from SAMMPRIS, 446 had reported lipoprotein(a) and LDL levels reported at follow-up and were therefore included. The median LDL was 101 mg/dl (IQR 77-130). There was no significant change in lipoprotein(a) at the first follow-up although low-density lipoprotein (LDL) levels fell significantly (relative difference -22%, IQR -38% to 0%). In adjusted Cox proportional hazards regression, every 1% change in LDL by the time of first follow-up was associated with a 0.9% relative reduction in the composite endpoint (adjusted hazard ratio [aHR] 1.009, 95% confidence interval [CI] 1.002 - 1.015). Assuming modest, average, and high projected effects of PCSK9i (40%, 60%, and 80% reduction in LDL), with half of SAMMPRIS patients having been treated, PCSK9i use could reduce outcome events by 18.1%, 24.6%, and 30.1%. With all SAMMPRIS patients having been treated, assuming an average PCSK9i effect, the primary outcome could be reduced by 43.6%.
Conclusions: Even with minimal gains from PCSK9i with stroke due to ICAD, atherosclerotic vascular events following stroke due to ICAD could be reduced significantly.
Methods: We conducted a secondary analysis of the SAMMPRIS clinical trial to estimate the association between changes in LDL and a composite outcome of first ischemic stroke, myocardial infarction, or death. Estimates were assessed using an adjusted Cox proportional hazards model accounting for age, sex, race, Hispanic ethnicity, baseline LDL level, vascular comorbidities, and use of intracranial stenting. We applied relative LDL reduction estimates from meta-analyzed trial data evaluating the effect of PCSK9i versus placebo among statin users with atherosclerotic vascular disease to project adjusted incidence rate differences of the primary outcome observed in SAMMPRIS with an equivalent LDL reduction. Semiparametric Cox proportional hazards models estimated the annualized relative risk of primary events if PCSK9i were used with aggressive risk factor modification for stroke due to ICAD.
Results: Of the 451 patients from SAMMPRIS, 446 had reported lipoprotein(a) and LDL levels reported at follow-up and were therefore included. The median LDL was 101 mg/dl (IQR 77-130). There was no significant change in lipoprotein(a) at the first follow-up although low-density lipoprotein (LDL) levels fell significantly (relative difference -22%, IQR -38% to 0%). In adjusted Cox proportional hazards regression, every 1% change in LDL by the time of first follow-up was associated with a 0.9% relative reduction in the composite endpoint (adjusted hazard ratio [aHR] 1.009, 95% confidence interval [CI] 1.002 - 1.015). Assuming modest, average, and high projected effects of PCSK9i (40%, 60%, and 80% reduction in LDL), with half of SAMMPRIS patients having been treated, PCSK9i use could reduce outcome events by 18.1%, 24.6%, and 30.1%. With all SAMMPRIS patients having been treated, assuming an average PCSK9i effect, the primary outcome could be reduced by 43.6%.
Conclusions: Even with minimal gains from PCSK9i with stroke due to ICAD, atherosclerotic vascular events following stroke due to ICAD could be reduced significantly.
More abstracts on this topic:
Abdominal Aortic Perivascular Adipose Tissue Lipolysis Is Activated In Hypertensive Dahl SS Rats Fed a High-Fat Diet
Chirivi Miguel, Rendon Javier, Lauver Adam, Fink Gregory, Watts Stephanie, Contreras Andres
Atherosclerotic Cardiovascular Disease Risk Management in a Primary Care Residency ClinicManalo Kathryn, Tieliwaerdi Xiarepati, Jackson Megan, Arrigo Alexis, Mascara Mariah, Maharjan Srijana, Gadani Mrudula
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)