Final ID: TMP67
Validation and Modification of the Simplified Edinburgh CT Criteria in Asian Lobar Intracerebral Hemorrhage: The Proposal of Asian CT Criteria for Cerebral Amyloid Angiopathy
Abstract Body: Background and Objective. The simplified Edinburgh CT criteria allowed a diagnosis of cerebral amyloid angiopathy (CAA) in spontaneous lobar intracerebral hemorrhage (ICH) for patients with limited accessibilities to MRI. However, its applicability to Asian populations remains uncertain. This study evaluated the diagnostic accuracy of the simplified Edinburgh CT criteria in Asian lobar ICH and to propose modifications if the performance is suboptimal.
Methods. We analyzed patients with spontaneous lobar ICH (≥ 50 years) from 2015 to 2022 who underwent an acute CT and an MRI. The CT images were assessed according to the LINCHPIN CT RATING FORM. Demographic and imaging parameters were compared between probable CAA and non-CAA groups with modified Boston criteria as reference standards, and were selected to establish a logistic regression model. The modified version of CT criteria was evaluated by diagnostic accuracy, inter-rater reliability and decision curve analysis.
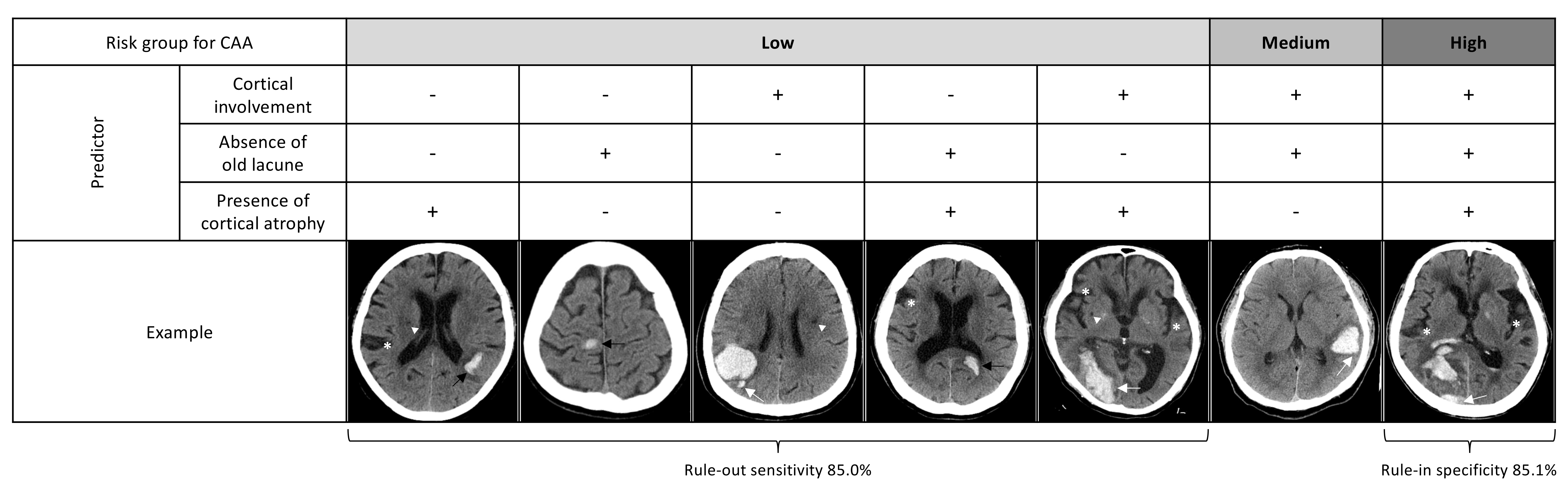
Results. A total of 87 lobar ICHs were included (ICH volume 20.1 [10.0-39.9] ml, 46.0% probable CAA). The presence of subarachnoid hemorrhage (SAH, 47.5% vs 21.3%, p=0.010), but not finger-like projection (FLP, 42.5% vs 23.4%, p=0.057), showed significant difference between probable CAA and non-CAA groups. The simplified Edinburgh CT criteria yielded only moderate diagnostic accuracy for CAA (AUC 0.66). To enhance the diagnostic performance, we identified additional CT markers that are related to CAA including cortical atrophy and deep atrophy; absent old striatocapsular insult, old lacune or vascular lesions (all p<0.05). The hematoma in CAA tended to be less oval, had more irregular borders and variable density, and almost always reached the cortex (all p<0.05). Accordingly, we developed the new criteria that incorporated hematoma cortical involvement, absence of old lacune, and presence of cortical atrophy in predicting probable CAA. All three markers showed excellent inter-rater reliability. The updated criteria yielded good AUC of 0.843 (0.759-0.927) without evidence of poor calibration, and provided the rule-in specificity of 85.1% and the rule-out sensitivity of 85.0%. Decision curve analysis supported the clinical net benefit.
Conclusions. The diagnostic accuracy of simplified Edinburgh CT criteria was suboptimal in Asians. We proposed the Asian version using CT markers of cortical involvement, absence of old lacune, and presence of cortical atrophy. External validation is warranted.
Methods. We analyzed patients with spontaneous lobar ICH (≥ 50 years) from 2015 to 2022 who underwent an acute CT and an MRI. The CT images were assessed according to the LINCHPIN CT RATING FORM. Demographic and imaging parameters were compared between probable CAA and non-CAA groups with modified Boston criteria as reference standards, and were selected to establish a logistic regression model. The modified version of CT criteria was evaluated by diagnostic accuracy, inter-rater reliability and decision curve analysis.
Results. A total of 87 lobar ICHs were included (ICH volume 20.1 [10.0-39.9] ml, 46.0% probable CAA). The presence of subarachnoid hemorrhage (SAH, 47.5% vs 21.3%, p=0.010), but not finger-like projection (FLP, 42.5% vs 23.4%, p=0.057), showed significant difference between probable CAA and non-CAA groups. The simplified Edinburgh CT criteria yielded only moderate diagnostic accuracy for CAA (AUC 0.66). To enhance the diagnostic performance, we identified additional CT markers that are related to CAA including cortical atrophy and deep atrophy; absent old striatocapsular insult, old lacune or vascular lesions (all p<0.05). The hematoma in CAA tended to be less oval, had more irregular borders and variable density, and almost always reached the cortex (all p<0.05). Accordingly, we developed the new criteria that incorporated hematoma cortical involvement, absence of old lacune, and presence of cortical atrophy in predicting probable CAA. All three markers showed excellent inter-rater reliability. The updated criteria yielded good AUC of 0.843 (0.759-0.927) without evidence of poor calibration, and provided the rule-in specificity of 85.1% and the rule-out sensitivity of 85.0%. Decision curve analysis supported the clinical net benefit.
Conclusions. The diagnostic accuracy of simplified Edinburgh CT criteria was suboptimal in Asians. We proposed the Asian version using CT markers of cortical involvement, absence of old lacune, and presence of cortical atrophy. External validation is warranted.
More abstracts on this topic:
AI-CVD vs. PREVENT for Predicting Incident Heart Failure: The Multi-Ethnic Study of Atherosclerosis (MESA)
Naghavi Morteza, Mirjalili Seyed Reza, Atlas Kyle, Zhang Chenyu, Reeves Anthony, Azimi Amir, Wong Nathan
Artificial Intelligence Based CCTA to Assess Sex-Based Differences in Coronary Atherosclerosis with Low Clinical Atheroma VolumeD'costa Zoee, Karlsberg Ronald, Cho Geoffrey
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)