Final ID: WP286
MRI-derived Pressure Ratio for Stroke Risk Assessment of Symptomatic Intracranial Atherosclerotic Stenosis
Abstract Body: Background: Hemodynamic evaluation is crucial in assessing stroke risk in patients with symptomatic intracranial atherosclerotic stenosis (sICAS). A new CFD model based on high-resolution MRI and phase-contrast MR angiography was developed to calculate translesional pressure ratio, called MRI-derived pressure ratio (MPR).
Purpose: We plan to conduct two studies to assess the diagnostic accuracy of MPR in detecting insufficient brain perfusion and its predictive value for clinical outcomes in sICAS patients.
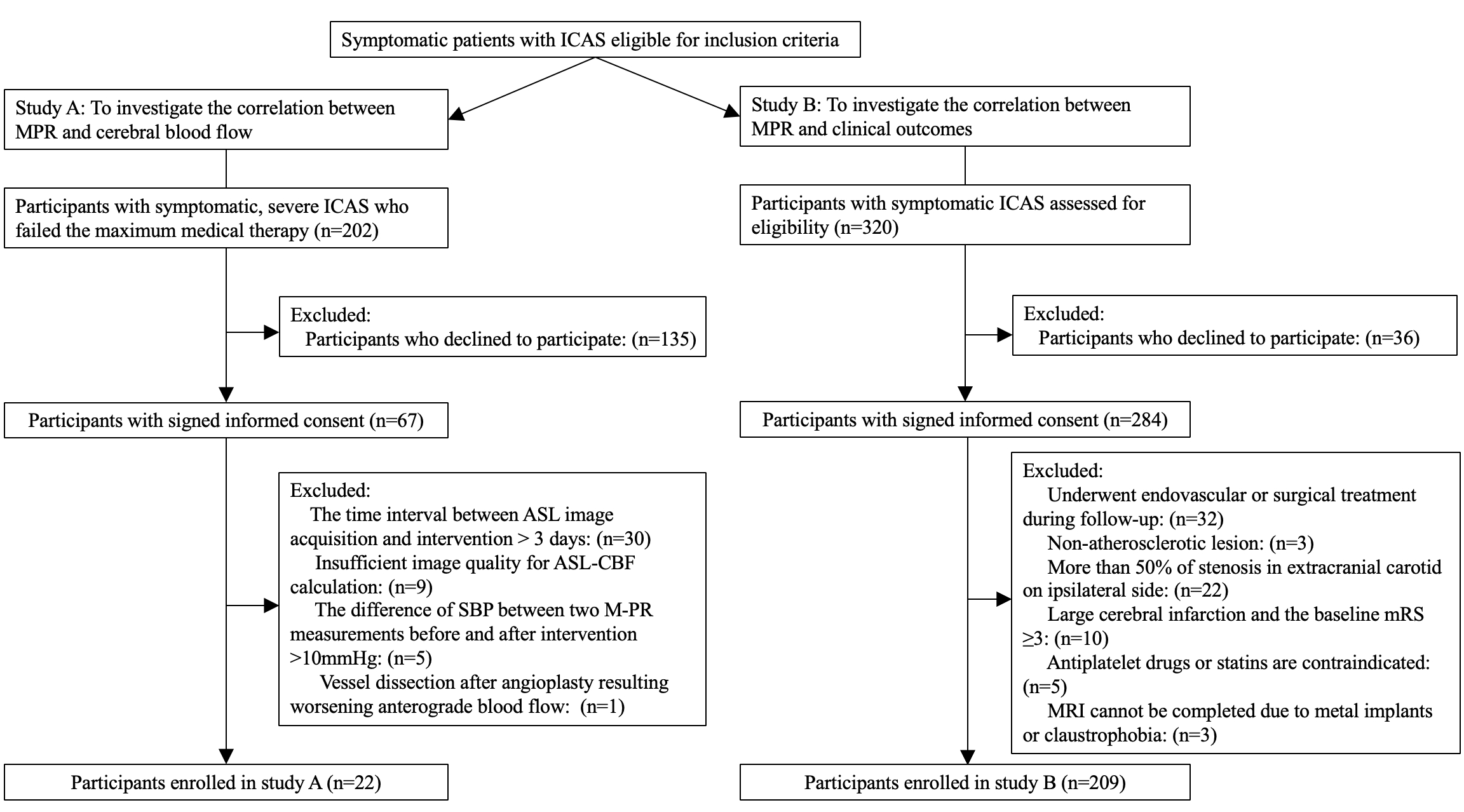
Methods: In the first study, sICAS patients who underwent percutaneous transluminal angioplasty and stenting (PTAS) were prospectively screened, with an arterial spin labeling-derived relative cerebral blood flow ratio (rCBF) of < 0.9 before PTAS. MPR (the ratio of poststenotic to prestenotic pressure) was calculated and collected before and after PTAS. If postoperative rCBF returned to normal (rCBF ≥ 0.9), the preoperative MPR was considered indicative of hemodynamic impairment, while the postoperative value was no. In the second study, patients with sICAS were prospectively enrolled and followed for one year under optimal medical treatment. MPR was assessed and recorded before enrollment. The primary outcome was a composite of recurrent ischemic stroke or TIA within the same arterial territory over one year.
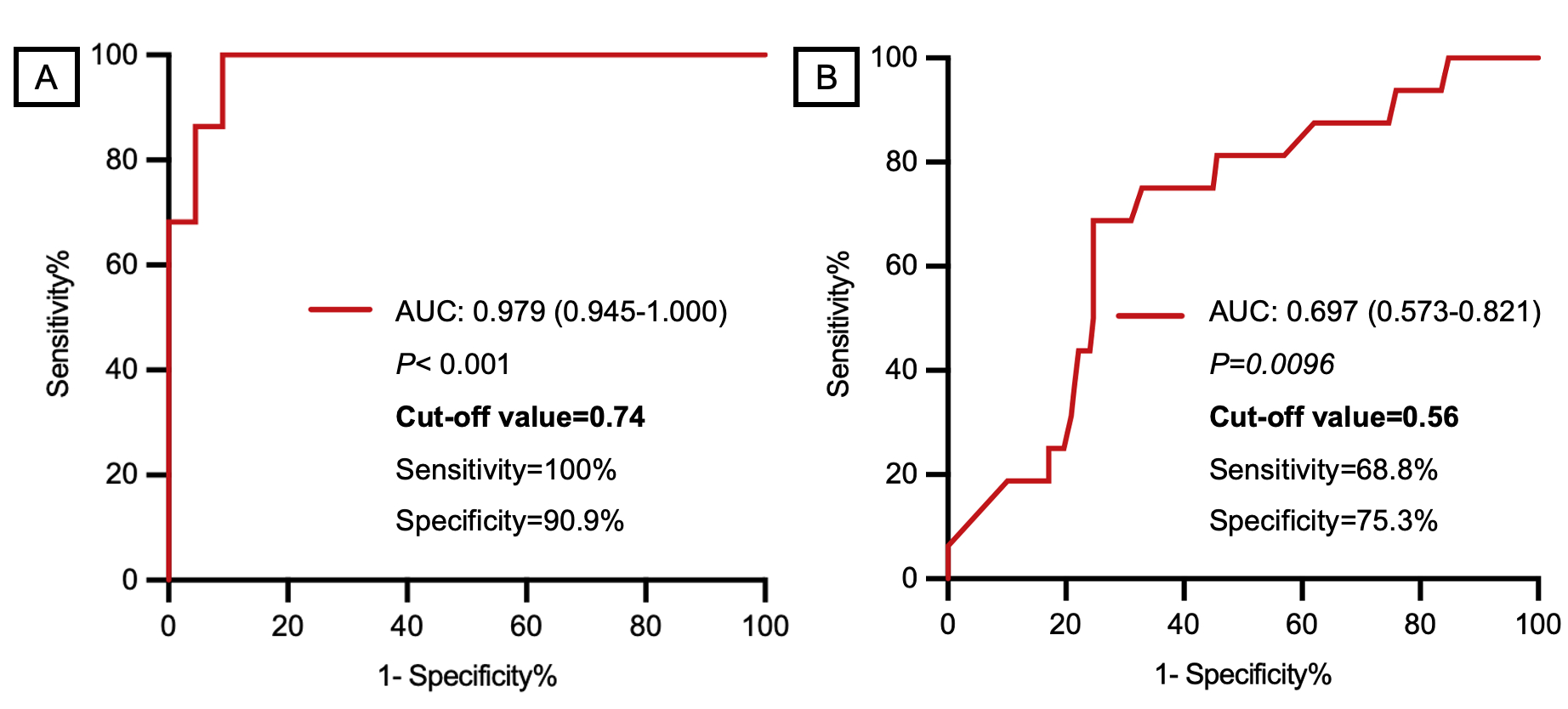
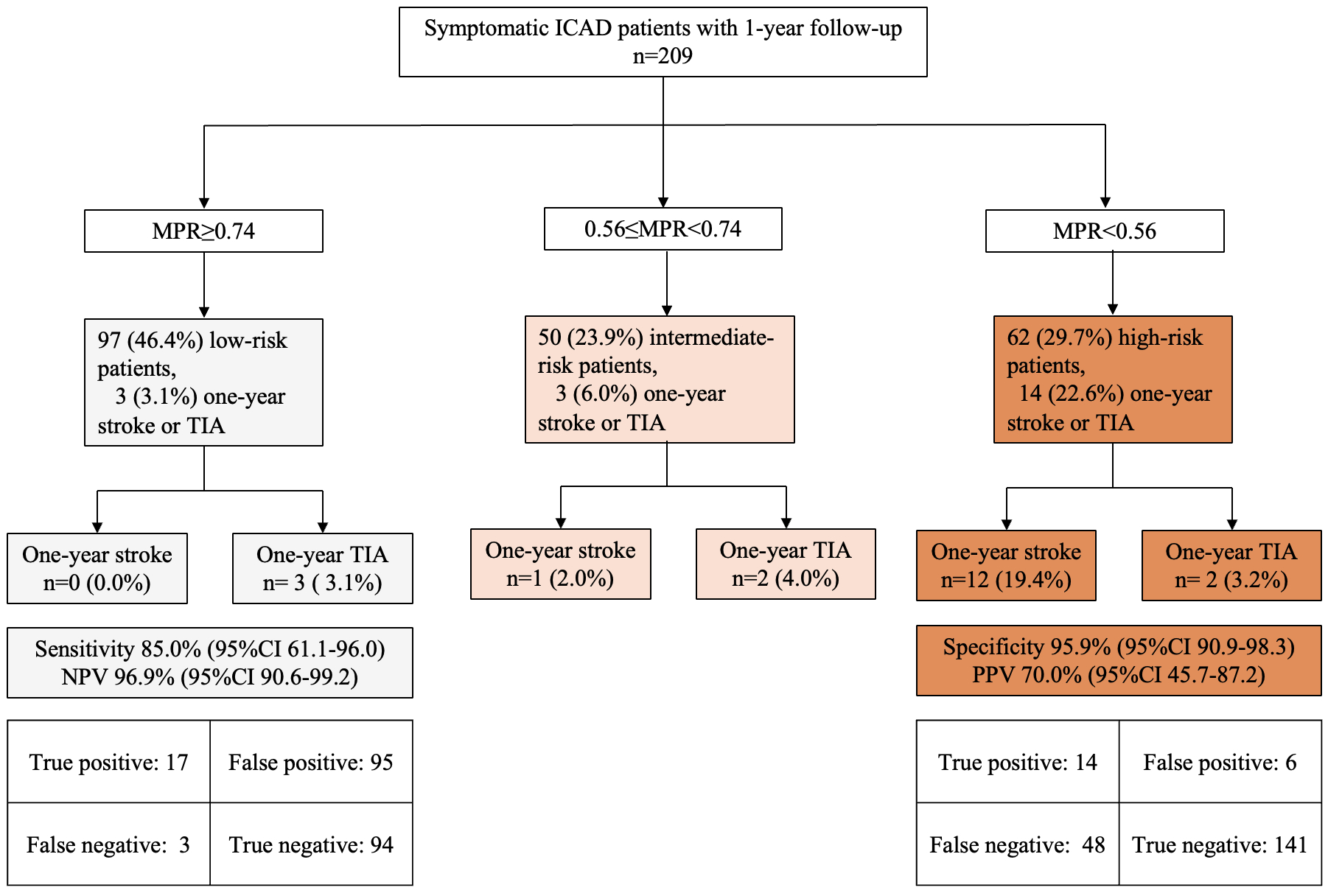
Results: In the first study, involving 22 patients (median age = 53 years, 81.8% males), MPR increased from 0.51 to 0.86 after PTAS. Cut-off values of MPR<0.74 identified as indicators of hemodynamic impairment. In the second study, 209 patients (median age = 55.0 years, 63.2% males) were included. Twenty patients (9.6%) experienced ischemic stroke or TIA during the one-year follow-up. Cut-off values of MPR < 0.56 was identified to best predict recurrent stroke or TIA. Multivariate logistic regression revealed that MPR (adjusted OR = 0.096, 95% CI = 0.013-0.71) was independently associated with the primary outcome. Next, patients were divided into three groups based on two cut-off values: low-risk (MPR≥0.74), intermediate-risk (0.56≤MPR<0.74), and high-risk (MPR<0.56). The one-year risk of stroke/TIA was significantly higher in the high-risk group compared to the low-risk (22.6% vs 3.1%, P<0.001) and intermediate-risk groups (22.6% vs 6.0%, P=0.023).
Conclusions: This study demonstrates that MPR is a reliable metric for risk stratification in sICAS patients. Future randomized trials are necessary to validate clinical decision-making guided by MPR.
Purpose: We plan to conduct two studies to assess the diagnostic accuracy of MPR in detecting insufficient brain perfusion and its predictive value for clinical outcomes in sICAS patients.
Methods: In the first study, sICAS patients who underwent percutaneous transluminal angioplasty and stenting (PTAS) were prospectively screened, with an arterial spin labeling-derived relative cerebral blood flow ratio (rCBF) of < 0.9 before PTAS. MPR (the ratio of poststenotic to prestenotic pressure) was calculated and collected before and after PTAS. If postoperative rCBF returned to normal (rCBF ≥ 0.9), the preoperative MPR was considered indicative of hemodynamic impairment, while the postoperative value was no. In the second study, patients with sICAS were prospectively enrolled and followed for one year under optimal medical treatment. MPR was assessed and recorded before enrollment. The primary outcome was a composite of recurrent ischemic stroke or TIA within the same arterial territory over one year.
Results: In the first study, involving 22 patients (median age = 53 years, 81.8% males), MPR increased from 0.51 to 0.86 after PTAS. Cut-off values of MPR<0.74 identified as indicators of hemodynamic impairment. In the second study, 209 patients (median age = 55.0 years, 63.2% males) were included. Twenty patients (9.6%) experienced ischemic stroke or TIA during the one-year follow-up. Cut-off values of MPR < 0.56 was identified to best predict recurrent stroke or TIA. Multivariate logistic regression revealed that MPR (adjusted OR = 0.096, 95% CI = 0.013-0.71) was independently associated with the primary outcome. Next, patients were divided into three groups based on two cut-off values: low-risk (MPR≥0.74), intermediate-risk (0.56≤MPR<0.74), and high-risk (MPR<0.56). The one-year risk of stroke/TIA was significantly higher in the high-risk group compared to the low-risk (22.6% vs 3.1%, P<0.001) and intermediate-risk groups (22.6% vs 6.0%, P=0.023).
Conclusions: This study demonstrates that MPR is a reliable metric for risk stratification in sICAS patients. Future randomized trials are necessary to validate clinical decision-making guided by MPR.
More abstracts on this topic:
Longitudinal Assessment of Vessel Wall Radiomics and Luminal Blood Flow During Evaluation of Intracranial Atherosclerotic Plaques
with intracranial arterial disease
Veeturi Sricharan, Pinter Nandor, Mecca Nicholas, Morrish Benjamin, Levy Elad, Siddiqui Adnan, Tutino Vincent
Impact of eicosapentaenoic acids and cilostazol in patientswith intracranial arterial disease
Takeishi Yusuke, Watanabe Yosuke, Matsuda Shingo, Okada Yoshio, Dowaki Ryosuke, Kuroki Kazuhiko
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)