Final ID: 145
New Oral Anticoagulant Therapy Versus Warfarin In Patients With Atrial Fibrillation And Previous Stroke or Transient Ischemic Attack. An Updated Meta-analysis.
Abstract Body: Background: Patients with atrial fibrillation (AF) and previous stroke or transient ischemic attack (TIA) are at high risk of recurrent stroke. Data regarding the efficacy and safety of new oral anticoagulant therapy (NOAC) compared to warfarin in patients with previous strokes are lacking.
Method: PubMed, Scopus and Cochrane databases were searched for both randomized controlled trials (RCTs) and non-randomized controlled trials (non-RCTs) that compared NOAC to warfarin in patients with AF and previous stroke or TIA and that reported the outcomes of cardiovascular death, death from any cause, disabling or fatal stroke, gastrointestinal major bleeding, hemorrhagic stroke, intracranial bleeding, major bleeding, overall stroke etc. Heterogeneity was examined using I2 statistics.
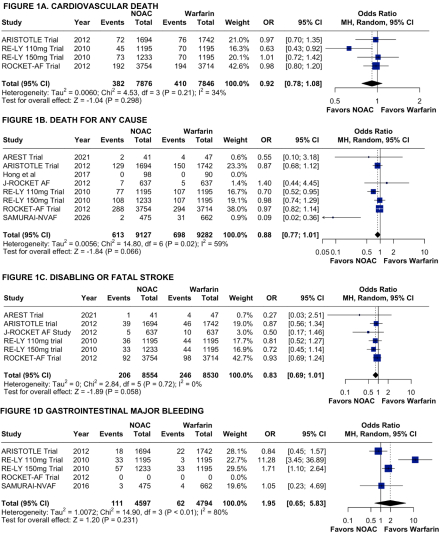
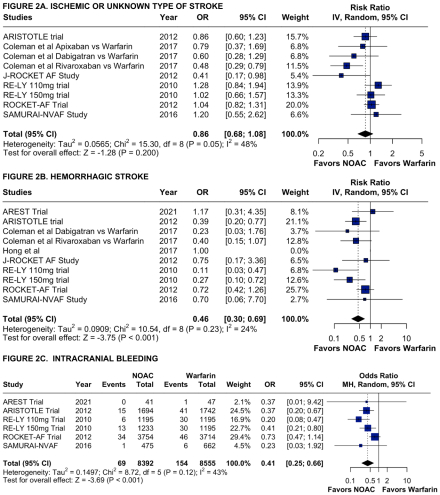
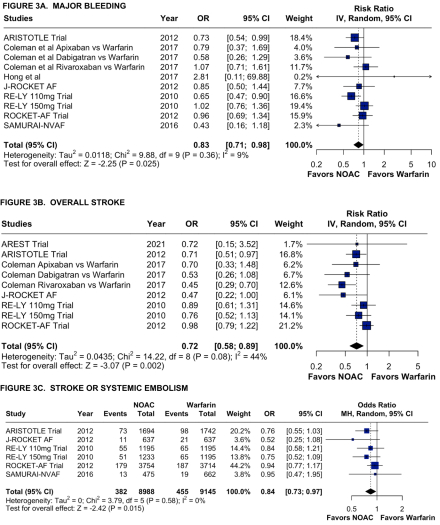
Results: We included 7 RCTs and 2 non-RCTs comparing NOAC to warfarin in patients with atrial fibrillation and previous stroke or TIA. The pooled results showed that cardiovascular death (4.9% vs 5.2% respectively; OR = 0.92; 95% CI [0.78, 1.08]; I2 = 34%; p = 0.298), death from any cause (6.7% vs 7.5% respectively; OR = 0.88; 95% CI [0.77, 1.01]; I2 = 59%; p = 0.066), disabling or fatal stroke (2.4% vs 2.9% respectively; OR = 0.83; 95% CI [0.69, 1.01]; I2 = 0%; p = 0.058), gastrointestinal major bleeding (2.4% vs 1.3% respectively; OR = 1.95; 95% CI [0.65, 5.83]; I2 = 80%; p = 0.231), and ischemic or unknown type of stroke (RR = 0.86; 95% CI [0.69, 1.08]; I2 = 48%; p = 0.200) are not statistically different between the NAOC group and warfarin group. However, hemorrhagic stroke (RR = 0.46; 95% CI [0.30, 0.69]; I2 = 24%; p < 0.001), intracranial bleeding (0.82% vs 1.8% respectively; OR = 0.41; 95% CI [0.25, 0.66]; I2 = 43%; p < 0.001), major bleeding (RR = 0.83; 95% CI [0.71, 0.98]; I2 = 9%; p = 0.025), overall stroke (RR = 0.72; 95% CI [0.58, 0.89]; I2 = 44%; p = 0.002) and stroke or systemic embolism (4.3% vs 5.0% respectively; OR = 0.84; 95% CI [0.73, 0.97]; I2 = 0%; p = 0.015) are significantly reduced in the NAOC group compared to the warfarin group.
Conclusion: In patients with atrial fibrillation and previous stroke or transient ischemic attack, treatment with NOAC did not show any significant difference compared with warfarin for outcomes of death from any cause, cardiovascular death, disabling or fatal stroke, and gastrointestinal major bleeding. NOAC reduces the risk of hemorrhagic stroke, intracranial bleeding, major bleeding, and overall stroke compared to warfarin.
Method: PubMed, Scopus and Cochrane databases were searched for both randomized controlled trials (RCTs) and non-randomized controlled trials (non-RCTs) that compared NOAC to warfarin in patients with AF and previous stroke or TIA and that reported the outcomes of cardiovascular death, death from any cause, disabling or fatal stroke, gastrointestinal major bleeding, hemorrhagic stroke, intracranial bleeding, major bleeding, overall stroke etc. Heterogeneity was examined using I2 statistics.
Results: We included 7 RCTs and 2 non-RCTs comparing NOAC to warfarin in patients with atrial fibrillation and previous stroke or TIA. The pooled results showed that cardiovascular death (4.9% vs 5.2% respectively; OR = 0.92; 95% CI [0.78, 1.08]; I2 = 34%; p = 0.298), death from any cause (6.7% vs 7.5% respectively; OR = 0.88; 95% CI [0.77, 1.01]; I2 = 59%; p = 0.066), disabling or fatal stroke (2.4% vs 2.9% respectively; OR = 0.83; 95% CI [0.69, 1.01]; I2 = 0%; p = 0.058), gastrointestinal major bleeding (2.4% vs 1.3% respectively; OR = 1.95; 95% CI [0.65, 5.83]; I2 = 80%; p = 0.231), and ischemic or unknown type of stroke (RR = 0.86; 95% CI [0.69, 1.08]; I2 = 48%; p = 0.200) are not statistically different between the NAOC group and warfarin group. However, hemorrhagic stroke (RR = 0.46; 95% CI [0.30, 0.69]; I2 = 24%; p < 0.001), intracranial bleeding (0.82% vs 1.8% respectively; OR = 0.41; 95% CI [0.25, 0.66]; I2 = 43%; p < 0.001), major bleeding (RR = 0.83; 95% CI [0.71, 0.98]; I2 = 9%; p = 0.025), overall stroke (RR = 0.72; 95% CI [0.58, 0.89]; I2 = 44%; p = 0.002) and stroke or systemic embolism (4.3% vs 5.0% respectively; OR = 0.84; 95% CI [0.73, 0.97]; I2 = 0%; p = 0.015) are significantly reduced in the NAOC group compared to the warfarin group.
Conclusion: In patients with atrial fibrillation and previous stroke or transient ischemic attack, treatment with NOAC did not show any significant difference compared with warfarin for outcomes of death from any cause, cardiovascular death, disabling or fatal stroke, and gastrointestinal major bleeding. NOAC reduces the risk of hemorrhagic stroke, intracranial bleeding, major bleeding, and overall stroke compared to warfarin.
More abstracts on this topic:
Ticagrelor Monotherapy in Patients with ACS Undergoing Coronary Stenting: An Updated Meta-Analysis of 3 Month versus 12 Month DAPT
Haseeb Mohsin, Shafiq Abdullah, Mungee Sudhir
A distinct clot transcriptomic signature is associated with atrial fibrillation-derived ischemic stroke in the INSIGHT RegistrySeah Carina, Rivet Dennis, Fraser Justin, Kellner Christopher, Devarajan Alex, Vicari James, Dabney Alan, Baltan Selva, Sohrabji Farida, Pennypacker Keith, Nanda Ashish, Woodward Britton
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)