Final ID: Mo2074
Safety and Efficacy with DOACs versus Warfarin in Patients with Atrial Fibrillation and Liver Cirrhosis: A Systematic Review and Meta-Analysis
Abstract Body (Do not enter title and authors here): Background
Atrial fibrillation (AF) is increasingly prevalent in patients with liver cirrhosis, which is associated with both bleeding and thromboembolism. Patients with cirrhosis have been excluded from randomized controlled trials on the efficacy and safety of anticoagulants in AF. We performed a systematic review to compare direct oral anticoagulants (DOACs) with warfarin in patients with AF and concomitant cirrhosis.
Methods
We systematically searched Pubmed and Embase from inception to the present. The primary outcome of interest was the hazard ratio of major bleeding. Secondary outcomes included gastrointestinal bleeding, all-cause bleeding, and ischemic stroke/systemic embolism[AN1] . Random effects models were used to calculate the weighted pooled hazard ratios for the outcomes. A two-tailed p<0.05 was considered statistically significant. Heterogeneity was assessed using the I2 index. Data analysis was performed using Revman version 5.4.1 (Cochrane).
Results
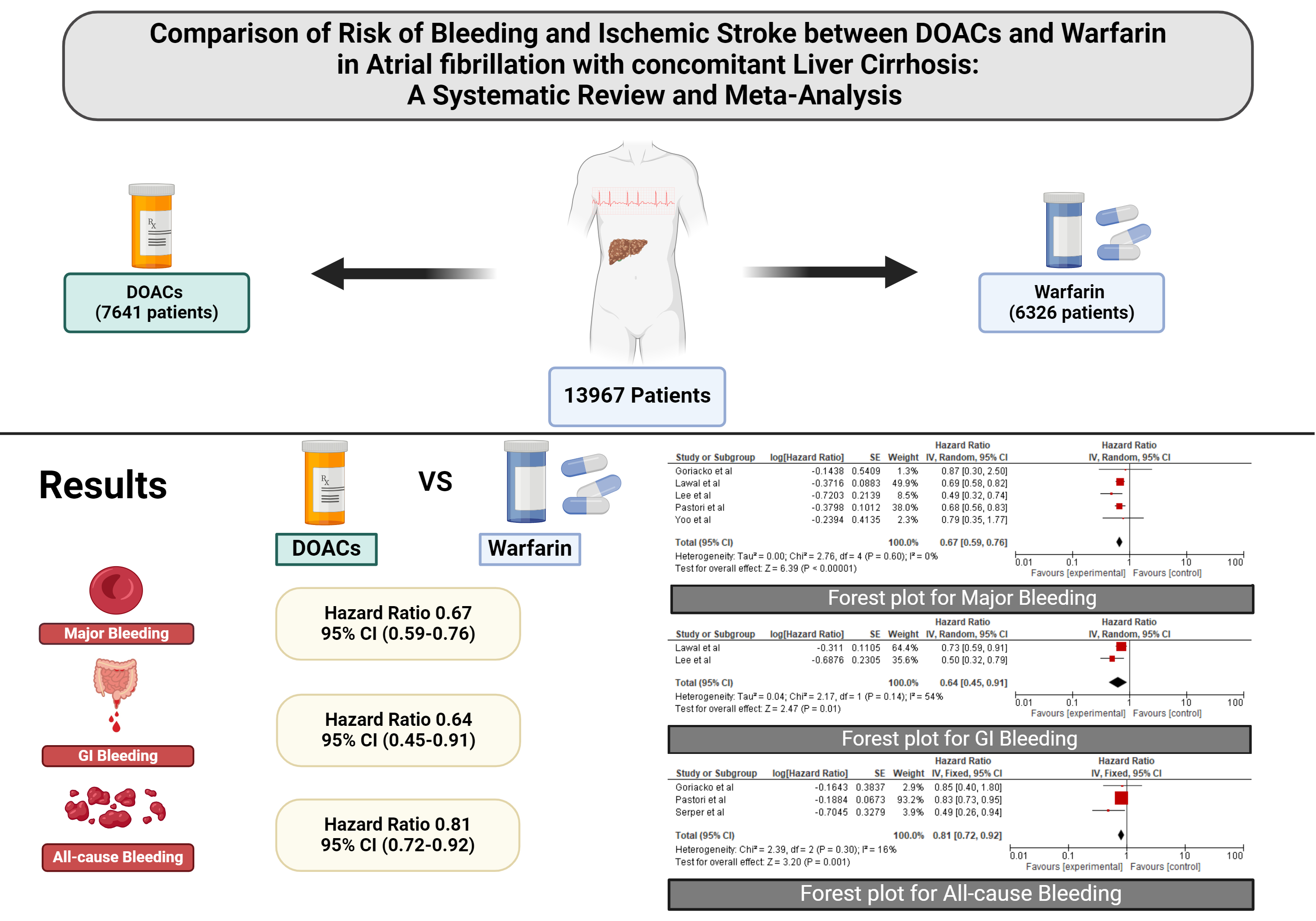
We included 5 non-randomized observational studies on patients with AF and cirrhosis (N=13,838). Among these, 7,641 were on DOACs and 6,326 were on warfarin. Men comprised 69.8% of the DOACs group and 69.1% of the warfarin group. The average age was 70.4±8.27 years in the DOACs group and 69.72±7.76 years in the warfarin group. Patients using antiplatelets comprised 26.7% of the DOAC group and 24.1% of the warfarin group. The mean HAS-BLED score was 3.00 in the DOACs group and 2.99 in the warfarin group. Compared to warfarin, DOACs used for AF in patients with cirrhosis were associated with a lower risk of major bleeding (HR 0.67, 95% CI [0.59, 0.76], I2=0%, p<0.00001), gastrointestinal bleeding (HR 0.64 [0.45, 0.91], I2=54%, p=0.01), and all-cause bleeding (HR 0.81 [0.72, 0.92], I2=16%, p=0.001). No difference was found in the incidence of ischemic stroke/systemic embolism (HR 1.09 [0.55, 2.15], I2=85%, p=0.81).
Conclusion
Our systematic review of non-randomized studies demonstrates that DOACs, as compared to warfarin, reduce the risk of bleeding in patients with AF and concomitant liver cirrhosis, without any difference in risk of stroke.
Atrial fibrillation (AF) is increasingly prevalent in patients with liver cirrhosis, which is associated with both bleeding and thromboembolism. Patients with cirrhosis have been excluded from randomized controlled trials on the efficacy and safety of anticoagulants in AF. We performed a systematic review to compare direct oral anticoagulants (DOACs) with warfarin in patients with AF and concomitant cirrhosis.
Methods
We systematically searched Pubmed and Embase from inception to the present. The primary outcome of interest was the hazard ratio of major bleeding. Secondary outcomes included gastrointestinal bleeding, all-cause bleeding, and ischemic stroke/systemic embolism[AN1] . Random effects models were used to calculate the weighted pooled hazard ratios for the outcomes. A two-tailed p<0.05 was considered statistically significant. Heterogeneity was assessed using the I2 index. Data analysis was performed using Revman version 5.4.1 (Cochrane).
Results
We included 5 non-randomized observational studies on patients with AF and cirrhosis (N=13,838). Among these, 7,641 were on DOACs and 6,326 were on warfarin. Men comprised 69.8% of the DOACs group and 69.1% of the warfarin group. The average age was 70.4±8.27 years in the DOACs group and 69.72±7.76 years in the warfarin group. Patients using antiplatelets comprised 26.7% of the DOAC group and 24.1% of the warfarin group. The mean HAS-BLED score was 3.00 in the DOACs group and 2.99 in the warfarin group. Compared to warfarin, DOACs used for AF in patients with cirrhosis were associated with a lower risk of major bleeding (HR 0.67, 95% CI [0.59, 0.76], I2=0%, p<0.00001), gastrointestinal bleeding (HR 0.64 [0.45, 0.91], I2=54%, p=0.01), and all-cause bleeding (HR 0.81 [0.72, 0.92], I2=16%, p=0.001). No difference was found in the incidence of ischemic stroke/systemic embolism (HR 1.09 [0.55, 2.15], I2=85%, p=0.81).
Conclusion
Our systematic review of non-randomized studies demonstrates that DOACs, as compared to warfarin, reduce the risk of bleeding in patients with AF and concomitant liver cirrhosis, without any difference in risk of stroke.
More abstracts on this topic:
A Hidden Threat: Trazodone-Induced Warfarin Failure Leading to Acute Mechanical Aortic Valve Thrombosis
Vogt Cody, Malik Saad, Pfirman Kristopher
A randomized controlled trial of antithrombotic therapy in ischemic stroke patients with non-valvular atrial fibrillation and atherosclerosis: The ATIS-NVAF trialOkazaki Shuhei, Uchida Kazutaka, Asakura Koko, Omae Katsuhiro, Yamamoto Haruko, Hirano Teruyuki, Toyoda Kazunori, Iguchi Yasuyuki, Noguchi Teruo, Okada Yasushi, Kitagawa Kazuo, Tanaka Kanta, Sakai Nobuyuki, Yamagami Hiroshi, Yazawa Yukako, Doijiri Ryosuke, Koga Masatoshi, Ihara Masafumi, Yamamoto Shiro, Kamiyama Kenji, Honda Yuko