Final ID: TAC156
Inhibition Of Macrophage Activation By Indole-3-acetic acid, a Metabolite Produced By The Gut Microbiota
Abstract Body: Endothelin-1 (ET-1), a 21-amino acid peptide, is the most potent vasoconstrictor in the body and is known for its strong inflammatory, mitogenic, and proliferative effects. Elevated levels of ET-1 stimulate macrophage cell surface ETAR and ETBR receptors, leading to their activation and triggering the production of reactive oxygen species (ROS), integrins, and inflammatory cytokines. This has in vivo implications in vascular inflammation, salt retention, kidney dysfunction, and sustained hypertension. Indole-3-acetic acid (IAA), a plant growth hormone and a metabolite of gut microbiota from dietary tryptophan, has been identified as a powerful inhibitor of blood pressure elevation and kidney dysfunction in Dahl salt-sensitive (DSS) hypertensive rats. This effect occurs through a unique dual-action mechanism: antagonism of both ET-1 receptors, ETAR and ETBR, and inhibition of endothelin-converting enzyme-1 (ECE-1). Since macrophages express both ET receptors and play a key role in the development of kidney dysfunction, the aim is to explore whether IAA can inhibit macrophage activation in vitro, which may potentially reduce kidney dysfunction in vivo.
Methods: In silico analyses, Cell culture, Western blotting (WB), Leukocyte adhesion assay, ROS assay.
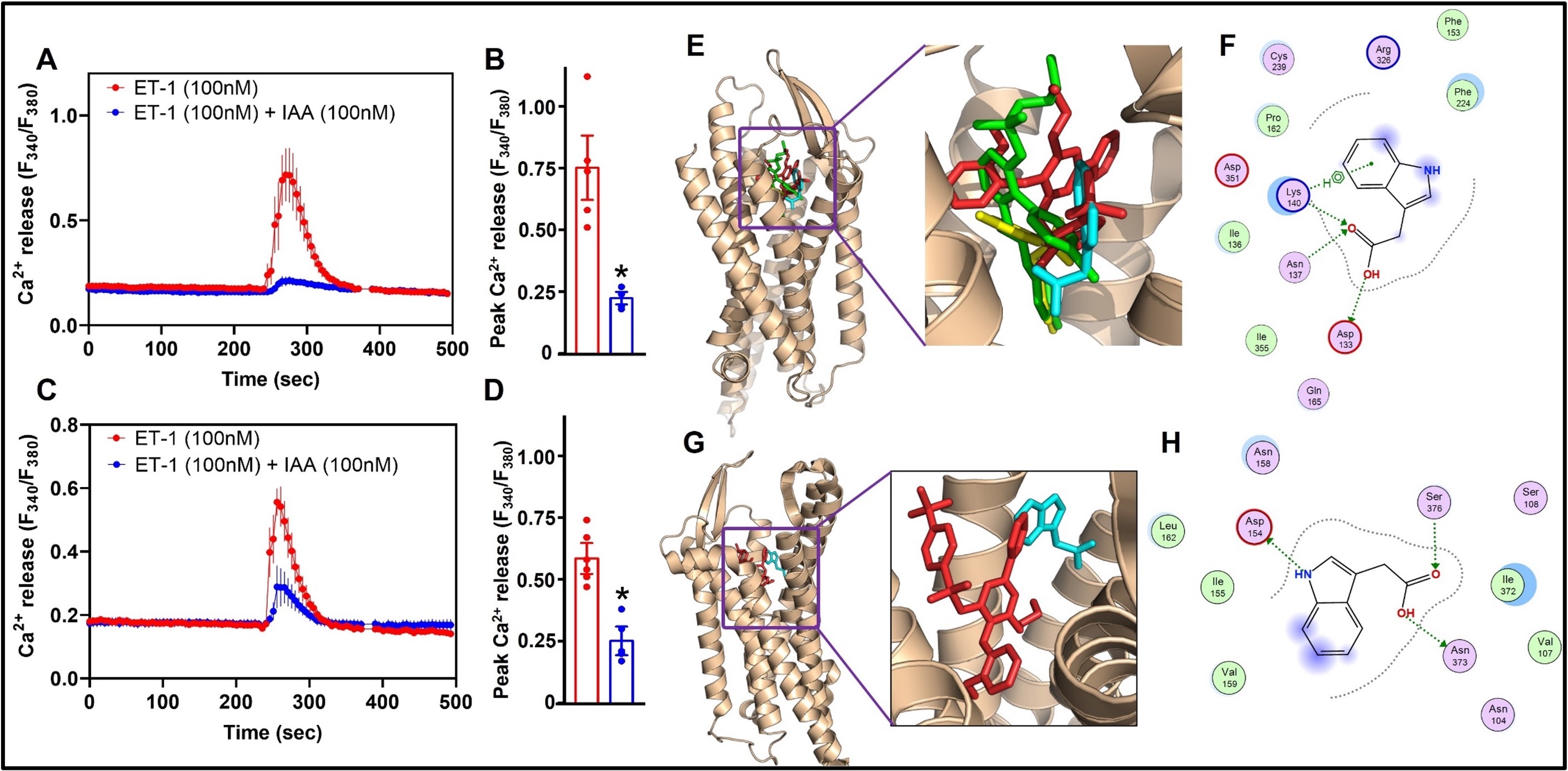
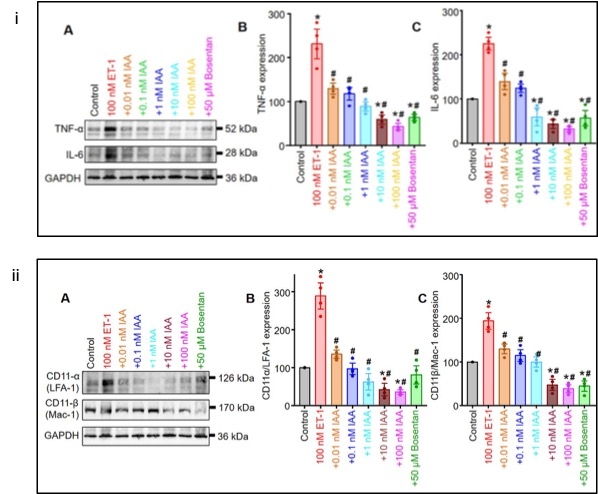
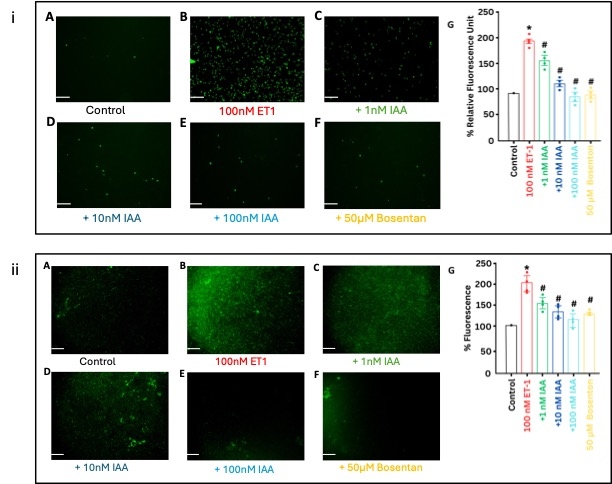
The Ca2+ imaging data reveals that IAA inhibits ET-1 stimulated, ETAR- and ETBR-mediated global increases in cytosolic Ca2+. In-silico analysis predicts that IAA interacts distinctly with the orthosteric binding pockets of both ETAR and ETBR, suggesting that IAA may act as a mixed antagonist. The Western blotting analysis shows both ETRs are present in the murine monocyte/macrophage cell line RAW264.7. ET-1 stimulates ROS, inflammatory cytokines, and integrins in RAW264.7 cells. Pretreatment with 100 nM IAA inhibits ET-1-mediated cytokine production, reducing IL-6, IL-17, and TNF-α by 190%, 130%, and 200%. IAA also suppresses overexpression of LFA-1 and MAC-1 integrins by 250% and 150%. Leukocyte adhesion assays demonstrate a 190% increase in macrophage attachment to endothelial cells with ET-1, reduced by 110% with 100 nM IAA. IAA reduces ET-1-induced ROS by 88%.
In conclusion, IAA inhibits ET-1 receptors in RAW264.7, suppressing activation. IAA could inhibit macrophage activation, reduce kidney infiltration, and mitigate damage - contributing to antihypertensive effects. Future studies will investigate ET-1 signaling in vasculature and macrophages in salt-sensitive hypertension, and IAA's efficacy in vivo.
Methods: In silico analyses, Cell culture, Western blotting (WB), Leukocyte adhesion assay, ROS assay.
The Ca2+ imaging data reveals that IAA inhibits ET-1 stimulated, ETAR- and ETBR-mediated global increases in cytosolic Ca2+. In-silico analysis predicts that IAA interacts distinctly with the orthosteric binding pockets of both ETAR and ETBR, suggesting that IAA may act as a mixed antagonist. The Western blotting analysis shows both ETRs are present in the murine monocyte/macrophage cell line RAW264.7. ET-1 stimulates ROS, inflammatory cytokines, and integrins in RAW264.7 cells. Pretreatment with 100 nM IAA inhibits ET-1-mediated cytokine production, reducing IL-6, IL-17, and TNF-α by 190%, 130%, and 200%. IAA also suppresses overexpression of LFA-1 and MAC-1 integrins by 250% and 150%. Leukocyte adhesion assays demonstrate a 190% increase in macrophage attachment to endothelial cells with ET-1, reduced by 110% with 100 nM IAA. IAA reduces ET-1-induced ROS by 88%.
In conclusion, IAA inhibits ET-1 receptors in RAW264.7, suppressing activation. IAA could inhibit macrophage activation, reduce kidney infiltration, and mitigate damage - contributing to antihypertensive effects. Future studies will investigate ET-1 signaling in vasculature and macrophages in salt-sensitive hypertension, and IAA's efficacy in vivo.
More abstracts on this topic:
A Loss-of-Function Missense Variant in ANGPTL3 Exerts Protective Effects Against Kidney Disease Risk
Zhang David, Ritchie Marylyn, Rader Daniel, Cuchel Marina
Contemporary Practice Patterns of Vasoactive Agents in Cardiogenic Shock: An Analysis of the AHA Cardiogenic Shock RegistryPatel Siddharth, Berg David, Bohula Erin, Palazzolo Michael, Krucoff Mitchell, Morrow David