Final ID: FR413
Beyond the Tumor: Persistent Hypertension and Delayed Cardiac Recovery Following Complex Paraganglioma Resection
Abstract Body: Case Presentation:
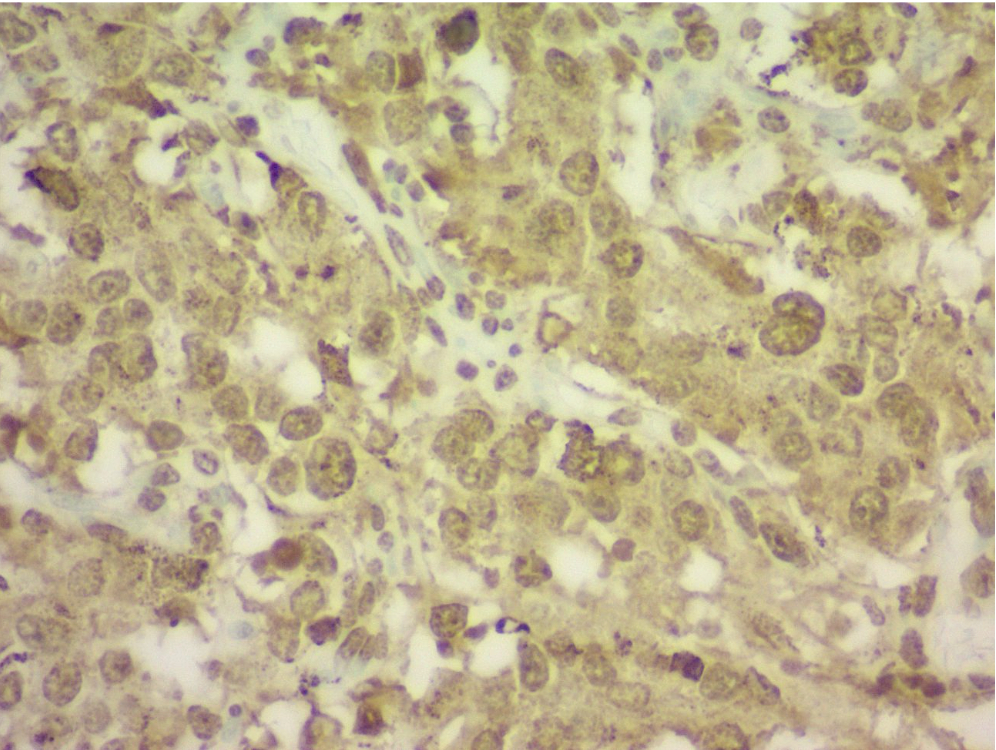
A 47-year-old African-American male with no known cardiac history presented with hypertensive emergency, acute heart failure (LVEF 30–35%), and multiorgan dysfunction. Imaging revealed a 14 cm extra-adrenal paraganglioma encasing the bilateral renal arteries, IVC, and adjacent vascular structures. Preoperative echocardiograms showed a progressive decline in LVEF from 45–50% to 30–35% over five months within diagnosis of paraganglioma. Surgical resection was performed, and histology confirmed paraganglioma. After resection, the patient continued to exhibit persistent hypertension despite adherence to antihypertensive therapy and lifestyle modification.
Differential Diagnosis:
Differentials included essential hypertension, renovascular hypertension, catecholamine-induced cardiomyopathy, and stress cardiomyopathy. The elevated catecholamines, vascular encasement, and classic symptoms confirmed a diagnosis of paraganglioma-associated secondary hypertension.
Treatment and Management:
Following resection, the patient was managed on losartan, carvedilol, prazosin, and nifedipine for blood pressure control, along with guideline-directed medical therapy for heart failure. He was discharged with a wearable defibrillator and referred for outpatient follow-up.
Outcome and Follow-Up:
He reported symptomatic improvement, and an LVEF was noted to improved to 45% after 3 weeks post resection. However, the patient remained severely hypertensive (SBP >180 mmHg) at multiple visits. He was compliant with therapy and lifestyle changes, but socioeconomic barriers limited access to further diagnostic workup and optimization.
Teaching Points:
This case highlights the complexity of managing catecholamine-induced cardiomyopathy, including potential for delayed cardiac recovery and persistent postoperative hypertension. Despite tumor resection and clinical stabilization, irreversible vascular and myocardial remodeling may contribute to long-term cardiovascular risk. Additionally, socioeconomic factors may limit optimal follow-up and secondary hypertension evaluation. Persistent hypertension after biochemical cure should not be underestimated and warrants aggressive, individualised outpatient management.
A 47-year-old African-American male with no known cardiac history presented with hypertensive emergency, acute heart failure (LVEF 30–35%), and multiorgan dysfunction. Imaging revealed a 14 cm extra-adrenal paraganglioma encasing the bilateral renal arteries, IVC, and adjacent vascular structures. Preoperative echocardiograms showed a progressive decline in LVEF from 45–50% to 30–35% over five months within diagnosis of paraganglioma. Surgical resection was performed, and histology confirmed paraganglioma. After resection, the patient continued to exhibit persistent hypertension despite adherence to antihypertensive therapy and lifestyle modification.
Differential Diagnosis:
Differentials included essential hypertension, renovascular hypertension, catecholamine-induced cardiomyopathy, and stress cardiomyopathy. The elevated catecholamines, vascular encasement, and classic symptoms confirmed a diagnosis of paraganglioma-associated secondary hypertension.
Treatment and Management:
Following resection, the patient was managed on losartan, carvedilol, prazosin, and nifedipine for blood pressure control, along with guideline-directed medical therapy for heart failure. He was discharged with a wearable defibrillator and referred for outpatient follow-up.
Outcome and Follow-Up:
He reported symptomatic improvement, and an LVEF was noted to improved to 45% after 3 weeks post resection. However, the patient remained severely hypertensive (SBP >180 mmHg) at multiple visits. He was compliant with therapy and lifestyle changes, but socioeconomic barriers limited access to further diagnostic workup and optimization.
Teaching Points:
This case highlights the complexity of managing catecholamine-induced cardiomyopathy, including potential for delayed cardiac recovery and persistent postoperative hypertension. Despite tumor resection and clinical stabilization, irreversible vascular and myocardial remodeling may contribute to long-term cardiovascular risk. Additionally, socioeconomic factors may limit optimal follow-up and secondary hypertension evaluation. Persistent hypertension after biochemical cure should not be underestimated and warrants aggressive, individualised outpatient management.
More abstracts on this topic:
A closed-loop system based on piezoelectric thin-film sensors and photothermal nanomaterials enables precise renal denervation for the treatment of hypertension
Liu Chengzhe, Zhou Liping, Yu Lilei
A Comparative Study Of Social Determinants, Hypertension, And Life Essential Factors In Alabama And Colorado From The 2021 Behavioral Risk Factor Surveillance SystemChukwunyere Chibuike, Owuor Kevin