Final ID: TH196
Three Decades of Change in Heart Failure Due to Hypertensive Renal Disease in the U.S.: Prevalence, Disability, and Disparities from 1990 to 2021
Abstract Body: Background:
Heart failure (HF) resulting from hypertensive renal disease (HRD) reflects a critical intersection of cardiovascular and renal pathologies. Despite its growing relevance, long-term epidemiologic trends of HF-HRD in the United States remain poorly quantified. This study aimed to assess temporal changes in prevalence and disability burden over the past three decades.
Methods:
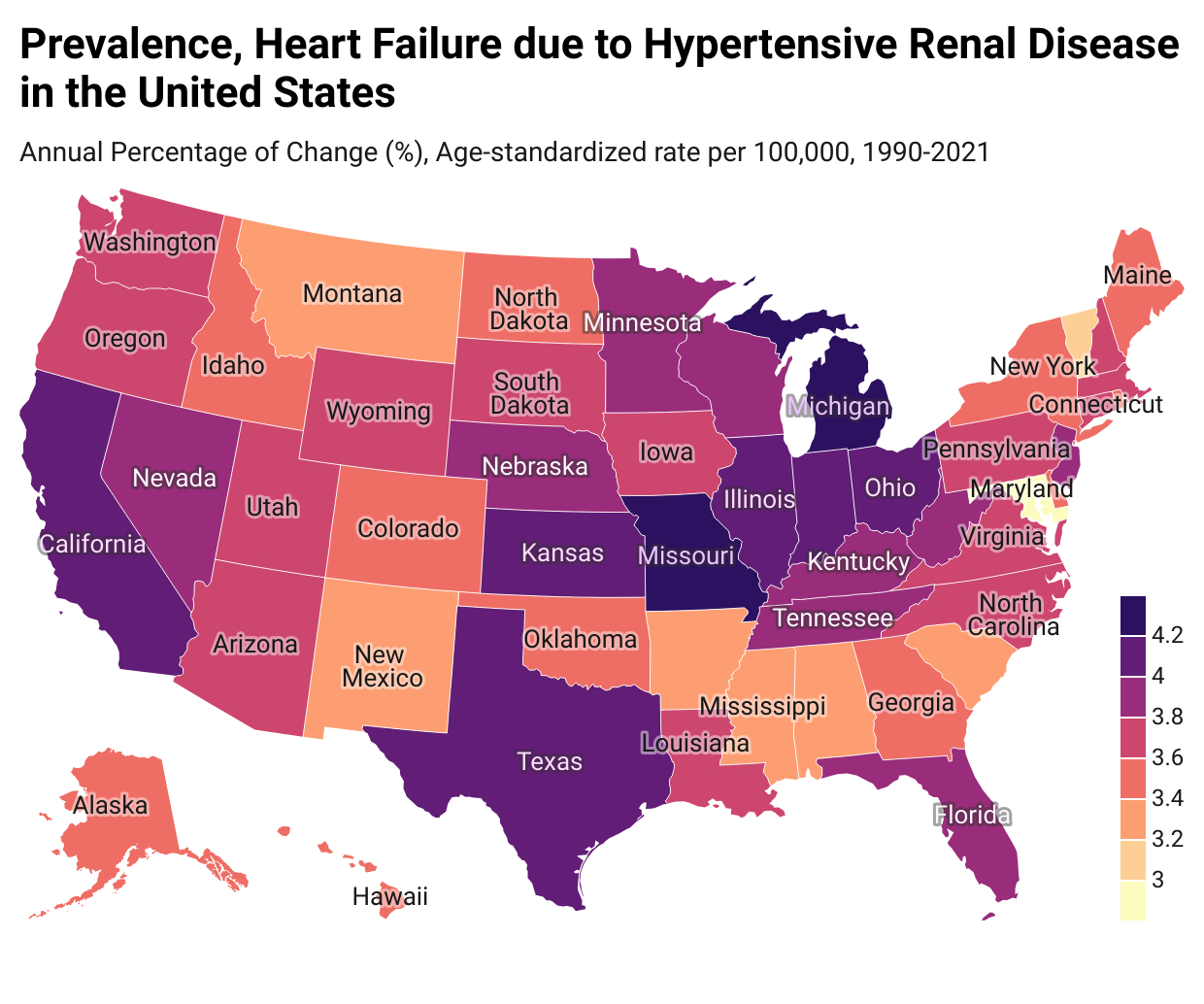
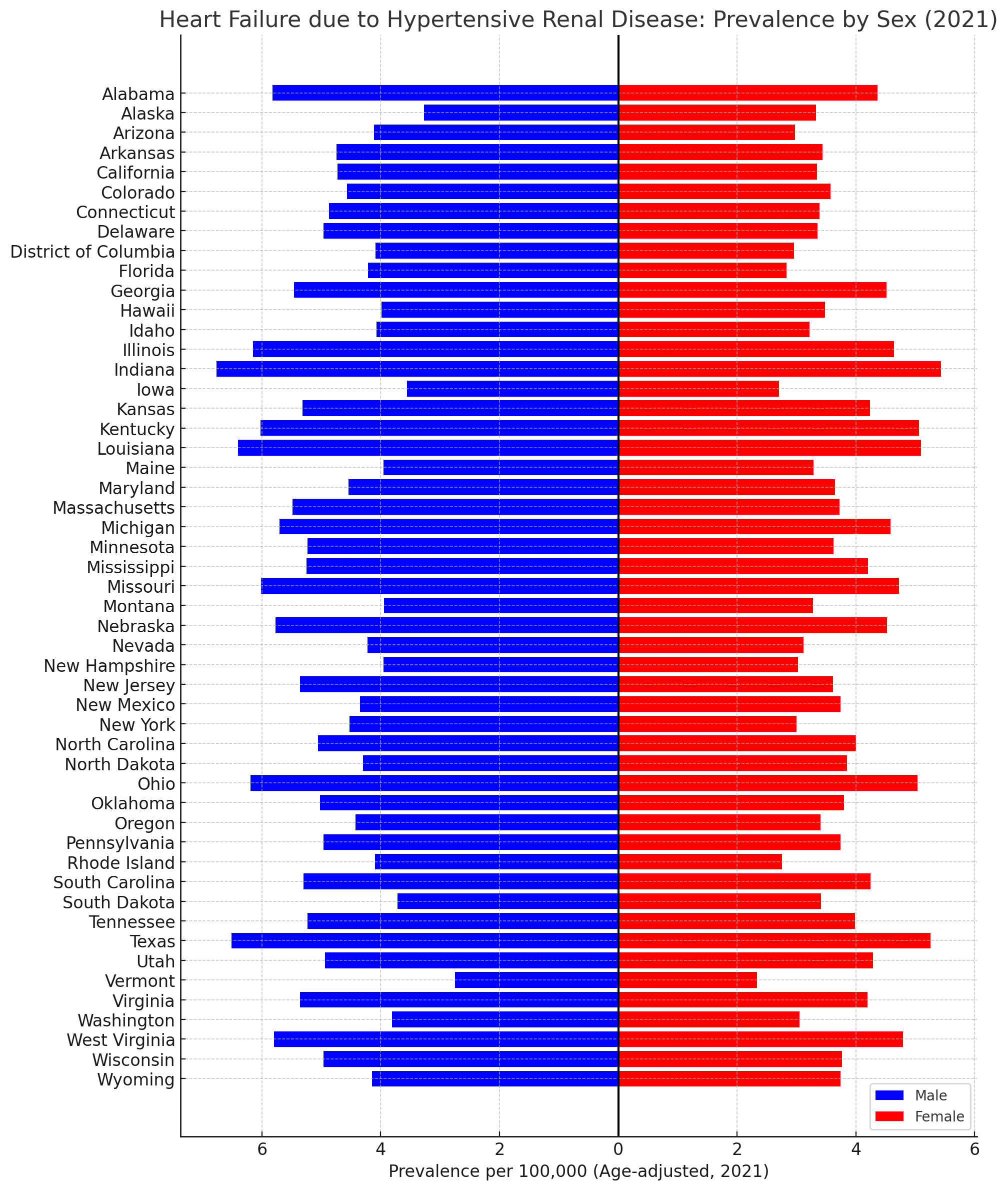
We utilized the Global Burden of Disease (GBD) 2021 framework to estimate age-standardized prevalence rates (ASPR, per 100,000) and years lived with disability (YLDs) attributable to HF due to HRD across U.S. states from 1990 to 2021. Estimates were stratified by age, sex, and geography, with 95% uncertainty intervals (UIs). Annualized percentage change (APC) was calculated using log-linear regression.
Results:
From 1990 to 2021, the total number of prevalent cases increased from 4,382 (UI: 3,162–5,892) to 26,532 (18,991–37,031), and YLDs rose from 565 (334–881) to 3,348 (2,004–5,341). ASPR escalated from 1.35 (0.99–1.76) to 4.40 (3.23–6.04). In 2021, Indiana recorded the highest ASPR at 5.98, followed by Texas (5.78) and Louisiana (5.64). Individuals aged ≥55 years bore the greatest burden (ASPR: 24.79), whereas the 20–54 age group had significantly lower rates (0.8). The highest total percentage change (TPC) was observed in those aged ≥95 years (315%) and 85–89 years (307%). Males experienced a steeper increase than females in both prevalence (579% vs 445%) and YLDs (564% vs 433%).
Conclusion:
The striking escalation in the prevalence and disability burden of HF-HRD across U.S. states—particularly among older adults and males—underscores an emerging cardio-renal crisis that has silently intensified over three decades. These findings call for a paradigm shift toward integrated surveillance and intervention models that bridge nephrology and cardiology. To curb this trajectory, future public health strategies must prioritize early screening in high-risk populations, address modifiable upstream factors such as hypertension control and kidney health literacy, and invest in state-level infrastructure capable of implementing tailored, age-specific prevention and management pathways.
Heart failure (HF) resulting from hypertensive renal disease (HRD) reflects a critical intersection of cardiovascular and renal pathologies. Despite its growing relevance, long-term epidemiologic trends of HF-HRD in the United States remain poorly quantified. This study aimed to assess temporal changes in prevalence and disability burden over the past three decades.
Methods:
We utilized the Global Burden of Disease (GBD) 2021 framework to estimate age-standardized prevalence rates (ASPR, per 100,000) and years lived with disability (YLDs) attributable to HF due to HRD across U.S. states from 1990 to 2021. Estimates were stratified by age, sex, and geography, with 95% uncertainty intervals (UIs). Annualized percentage change (APC) was calculated using log-linear regression.
Results:
From 1990 to 2021, the total number of prevalent cases increased from 4,382 (UI: 3,162–5,892) to 26,532 (18,991–37,031), and YLDs rose from 565 (334–881) to 3,348 (2,004–5,341). ASPR escalated from 1.35 (0.99–1.76) to 4.40 (3.23–6.04). In 2021, Indiana recorded the highest ASPR at 5.98, followed by Texas (5.78) and Louisiana (5.64). Individuals aged ≥55 years bore the greatest burden (ASPR: 24.79), whereas the 20–54 age group had significantly lower rates (0.8). The highest total percentage change (TPC) was observed in those aged ≥95 years (315%) and 85–89 years (307%). Males experienced a steeper increase than females in both prevalence (579% vs 445%) and YLDs (564% vs 433%).
Conclusion:
The striking escalation in the prevalence and disability burden of HF-HRD across U.S. states—particularly among older adults and males—underscores an emerging cardio-renal crisis that has silently intensified over three decades. These findings call for a paradigm shift toward integrated surveillance and intervention models that bridge nephrology and cardiology. To curb this trajectory, future public health strategies must prioritize early screening in high-risk populations, address modifiable upstream factors such as hypertension control and kidney health literacy, and invest in state-level infrastructure capable of implementing tailored, age-specific prevention and management pathways.
More abstracts on this topic:
Burden of Chronic Kidney Disease Due to Hypertension Attributable to Dietary Risk Factors: Global Trends and Regional Inequities (1990–2021)
Dudhat Kushal, Patel Ridham, Patel Juhi, Desai Hardik, Amin Vishrant, Patel Vishva, Zinzala Hardik, Patel Ker, Sakariya Dhrumil Chhaganbhai, Patel Kevin, Patel Kesar, Gopi Gokul, Sami Shahzad Ahmed
A Comparison of Characteristics and Outcomes in Patients with and without Adult Congenital Heart Disease Undergoing Catheter Ablation for Ventricular TachycardiaFutela Pragyat, Poddar Aastha, Kowlgi Gurukripa