Final ID: FR411
Hypertensive Crisis as a Presenting Sign of Paraneoplastic Cushing Syndrome in Recurrent Metastatic Small Cell Lung Cancer
Abstract Body: Case Summary
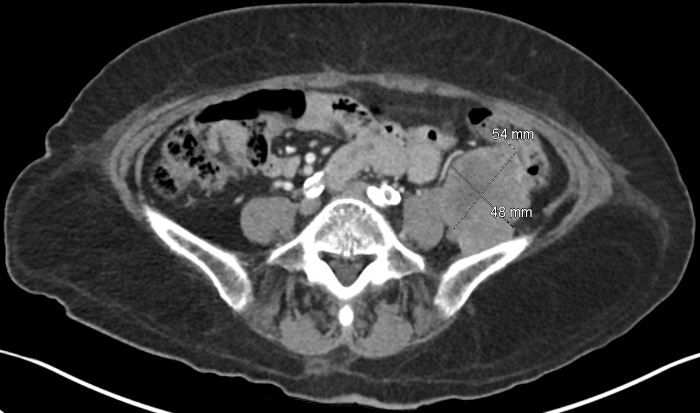
A 70 year old female with stage II hypertension, controlled type 2 diabetes, chronic hepatitis B, previously treated hepatitis C, benign right thyroid nodule, and small cell lung cancer (SCLC) in remission presented to the emergency room with 5 days of severe fatigue and hyperglycemia. Blood pressure (BP) was elevated to 201/123. Exam was notable for facial hyperpigmentation and right supraclavicular fullness. Labs showed hyperglycemia, hypokalemia, metabolic alkalosis, and leukocytosis. She was admitted for further evaluation. A prior colonoscopy had shown an ileocecal tubulovillous adenoma that could not be resected. Given this, she had a CT torso which showed increased size of her known right thyroid nodule, two new left adrenal nodules, and likely retroperitoneal metastatic disease.
Differential Diagnosis
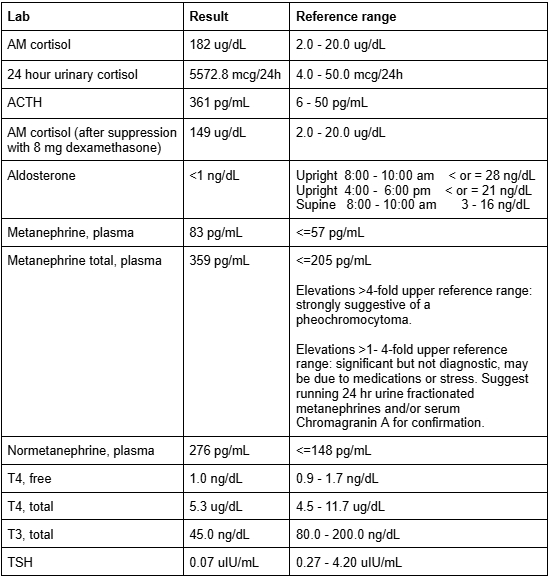
The differential included infection and endocrinopathy given metabolic derangements, with concern for malignancy given imaging findings. New adrenal nodules raised concern for Cushing syndrome (CS), primary aldosteronism, and pheochromocytoma. Infectious workup was notable only for urinary tract infection which was treated. Hepatitis B and C viral loads were undetectable. Additional lab testing shown in Figure 1 suggested ectopic ACTH secretion, concerning for paraneoplastic Cushing syndrome (PCS) in the setting of malignancy (possible recurrent SCLC versus new thyroid, adrenal, colon primary). MRI brain showed no pituitary tumor.
Treatment & Outcomes
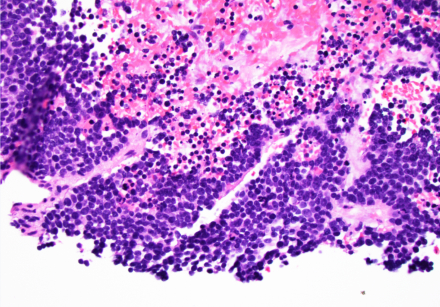
Hypertension was treated with amlodipine, labetalol, and spironolactone. Hypercortisolism was treated with metyrapone. Cortisol dropped from 182 to 4 ug/dL and BP improved to 120s-170s/60s-80s. Hyperglycemia was controlled with insulin. Biopsy results of the left retroperitoneal mass and right cervical lymph node were consistent with SCLC. She was started on palliative chemotherapy with carboplatin and etoposide.
Learning Points
This patient with hypertensive crisis and hyperglycemia was ultimately found to have PCS associated with metastatic SCLC. Prognosis of SCLC is poor with a median survival of 14 months, but is even worse at about 8 months for SCLC patients with PCS. Thus it is important to identify PCS early. Ectopic CS develops rapidly and is estimated to account for 5-10% of all CS cases. In a patient with a history of malignancy--especially SCLC--who presents with hypertensive crisis, it is important to maintain high suspicion of malignancy recurrence and paraneoplastic syndromes.
A 70 year old female with stage II hypertension, controlled type 2 diabetes, chronic hepatitis B, previously treated hepatitis C, benign right thyroid nodule, and small cell lung cancer (SCLC) in remission presented to the emergency room with 5 days of severe fatigue and hyperglycemia. Blood pressure (BP) was elevated to 201/123. Exam was notable for facial hyperpigmentation and right supraclavicular fullness. Labs showed hyperglycemia, hypokalemia, metabolic alkalosis, and leukocytosis. She was admitted for further evaluation. A prior colonoscopy had shown an ileocecal tubulovillous adenoma that could not be resected. Given this, she had a CT torso which showed increased size of her known right thyroid nodule, two new left adrenal nodules, and likely retroperitoneal metastatic disease.
Differential Diagnosis
The differential included infection and endocrinopathy given metabolic derangements, with concern for malignancy given imaging findings. New adrenal nodules raised concern for Cushing syndrome (CS), primary aldosteronism, and pheochromocytoma. Infectious workup was notable only for urinary tract infection which was treated. Hepatitis B and C viral loads were undetectable. Additional lab testing shown in Figure 1 suggested ectopic ACTH secretion, concerning for paraneoplastic Cushing syndrome (PCS) in the setting of malignancy (possible recurrent SCLC versus new thyroid, adrenal, colon primary). MRI brain showed no pituitary tumor.
Treatment & Outcomes
Hypertension was treated with amlodipine, labetalol, and spironolactone. Hypercortisolism was treated with metyrapone. Cortisol dropped from 182 to 4 ug/dL and BP improved to 120s-170s/60s-80s. Hyperglycemia was controlled with insulin. Biopsy results of the left retroperitoneal mass and right cervical lymph node were consistent with SCLC. She was started on palliative chemotherapy with carboplatin and etoposide.
Learning Points
This patient with hypertensive crisis and hyperglycemia was ultimately found to have PCS associated with metastatic SCLC. Prognosis of SCLC is poor with a median survival of 14 months, but is even worse at about 8 months for SCLC patients with PCS. Thus it is important to identify PCS early. Ectopic CS develops rapidly and is estimated to account for 5-10% of all CS cases. In a patient with a history of malignancy--especially SCLC--who presents with hypertensive crisis, it is important to maintain high suspicion of malignancy recurrence and paraneoplastic syndromes.
More abstracts on this topic:
Baseline Sex Hormone Binding Globulin Level Modifies Intensive Lifestyle Intervention Effect on Blood Pressure in Post-Menopausal Females
He Jiahuan Helen, Ma Jianqiao, Woodward Mark, Michos Erin, Oyeka Chigolum, Kalyani Rita, Clark Jeanne, Vaidya Dhananjay, Bennett Wendy
Impacts of perioperative cyclohexanone exposure on systemic inflammatory responseZheng Christie, Helmbrecht Hawley, Ellis Greg, Everett Allen, Graham David, Jantzie Lauren, Graham Eric, Kuiper Jordan