Final ID: 042
Microglia Depletion Mitigates Sympathetic Hyperactivity in Chronic Kidney Disease
Abstract Body: Introduction
Excess sympathetic nerve activity (SNA) is a key contributor to cardiovascular mortality in chronic kidney disease (CKD). However, the mechanisms driving excess SNA in CKD remain unclear. Emerging evidence links CKD to immune and cerebrovascular dysfunction. However, the role of microglia activation and subsequent neuroinflammation has never been explored.
Hypothesis
We hypothesize that microglial activation drives SNA in CKD.
Methods
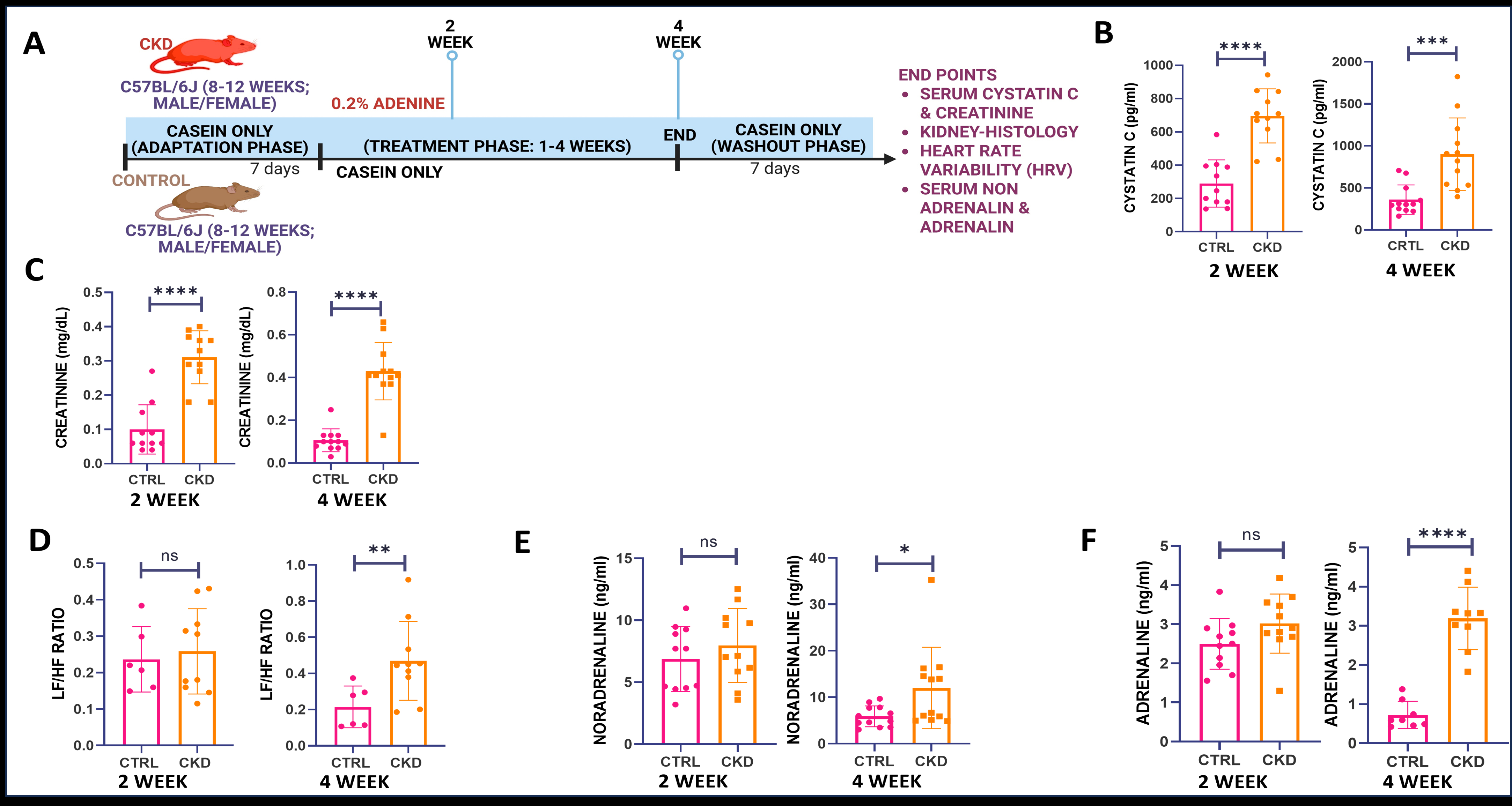
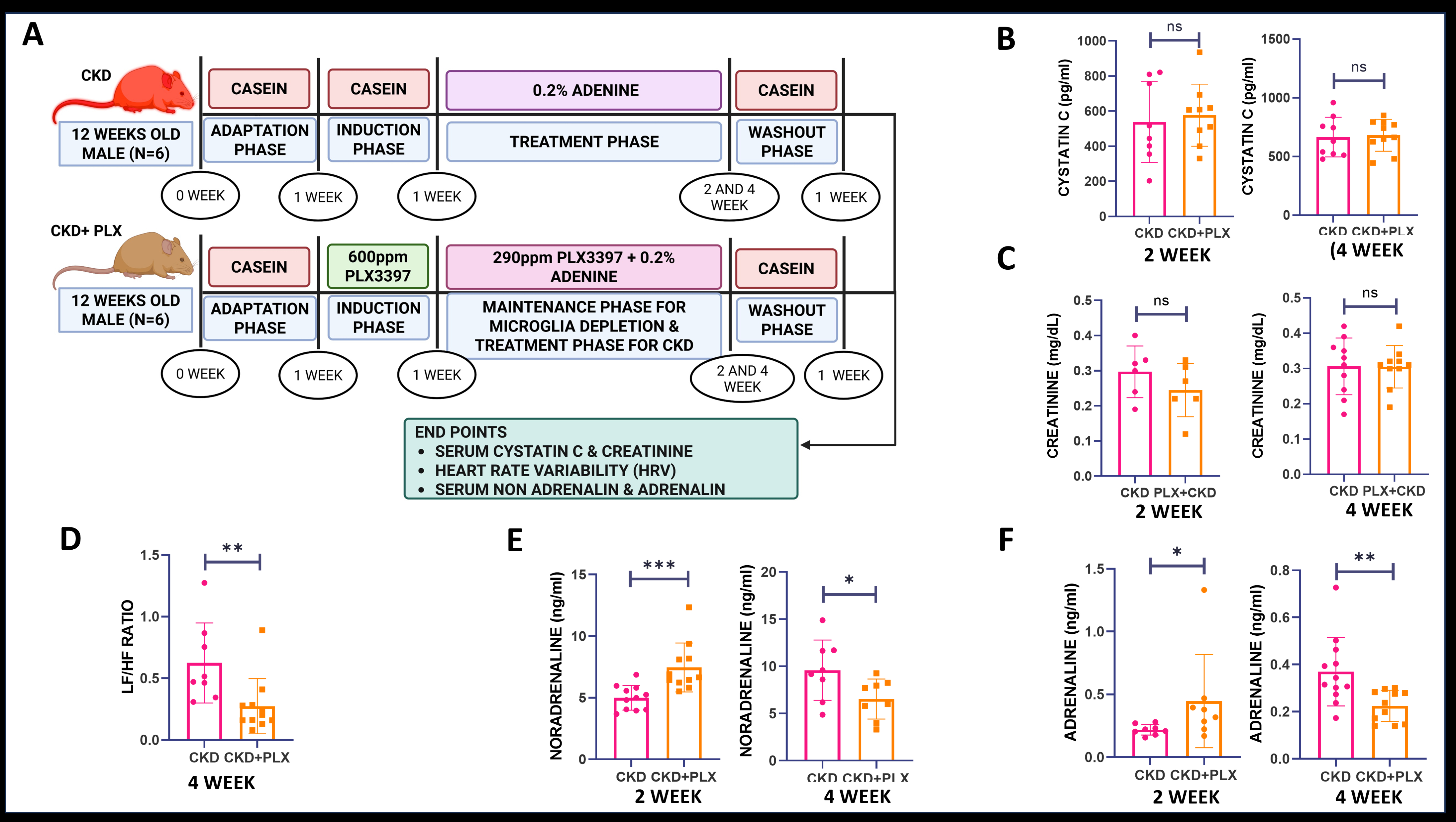
C57/BL6 mice (18-22gm, 8-11 weeks old) were randomized into groups as below: 0.2% adenine in casein (CKD), casein-only diet (Control), and 0.2% adenine + PLX 3397 (CKD and microglia depletion) for 2/4 weeks. Serum creatinine and cystatin C levels were used for assessing renal function. SNA was assessed by heart rate variability (Low Frequency/High-Frequency ratio) and catecholamine levels (ELISA). Cerebral perfusion and neurovascular coupling were assessed by Laser speckle contrast imaging (LSCI) and whisker stimulation test. Microglia phenotyping was done via flow cytometry. Neuroinflammation was evaluated by immunofluorescence and Luminex cytokine/chemokine array.
Results
The adenine diet induced significant CKD by 2 weeks. No significant differences in SNA were observed at 2 weeks but by 4 weeks SNA was significantly increased in CKD mice LF/HF ratio (0.46 ± 0.10 in CKD vs. 0.21 ± 0.05 in controls; P = 0.02). Importantly, LSCI and whisker stimulation testing revealed no significant changes in cerebral perfusion or neurovascular coupling between CKD and control groups. Changes in microglia were evident as early as 2 weeks with CKD mice showing an activated microglia phenotype (CD11b+ P2RY12+ CD86+ / CD11b+ P2RY12+ CD45HIGH CD86+) (P = 0.001/0.045). Microglial accumulation was particularly evident in brain regions governing sympathetic output. Microglia specific chemokine, RANTES significantly increase in CKD by 2/4 week. Notably, microglial depletion significantly reduced SNA in CKD mice by week 4 (LF/HF: 0.23 ± 0.11 in CKD + PLX3397 vs. 0.54 ± 0.22 in CKD alone; P = 0.0087).
Conclusion(s)
These findings demonstrate that CKD is associated with early microglial activation and subsequent neuroinflammation in brain regions regulating sympathetic tone. This neuroimmune activation precedes and contributes to heightened SNA, independent of neurovascular dysfunction. Microglial depletion attenuates sympathetic overactivity, identifying microglia as a mechanistic driver of excess SNA in CKD and a potential therapeutic target.
Excess sympathetic nerve activity (SNA) is a key contributor to cardiovascular mortality in chronic kidney disease (CKD). However, the mechanisms driving excess SNA in CKD remain unclear. Emerging evidence links CKD to immune and cerebrovascular dysfunction. However, the role of microglia activation and subsequent neuroinflammation has never been explored.
Hypothesis
We hypothesize that microglial activation drives SNA in CKD.
Methods
C57/BL6 mice (18-22gm, 8-11 weeks old) were randomized into groups as below: 0.2% adenine in casein (CKD), casein-only diet (Control), and 0.2% adenine + PLX 3397 (CKD and microglia depletion) for 2/4 weeks. Serum creatinine and cystatin C levels were used for assessing renal function. SNA was assessed by heart rate variability (Low Frequency/High-Frequency ratio) and catecholamine levels (ELISA). Cerebral perfusion and neurovascular coupling were assessed by Laser speckle contrast imaging (LSCI) and whisker stimulation test. Microglia phenotyping was done via flow cytometry. Neuroinflammation was evaluated by immunofluorescence and Luminex cytokine/chemokine array.
Results
The adenine diet induced significant CKD by 2 weeks. No significant differences in SNA were observed at 2 weeks but by 4 weeks SNA was significantly increased in CKD mice LF/HF ratio (0.46 ± 0.10 in CKD vs. 0.21 ± 0.05 in controls; P = 0.02). Importantly, LSCI and whisker stimulation testing revealed no significant changes in cerebral perfusion or neurovascular coupling between CKD and control groups. Changes in microglia were evident as early as 2 weeks with CKD mice showing an activated microglia phenotype (CD11b+ P2RY12+ CD86+ / CD11b+ P2RY12+ CD45HIGH CD86+) (P = 0.001/0.045). Microglial accumulation was particularly evident in brain regions governing sympathetic output. Microglia specific chemokine, RANTES significantly increase in CKD by 2/4 week. Notably, microglial depletion significantly reduced SNA in CKD mice by week 4 (LF/HF: 0.23 ± 0.11 in CKD + PLX3397 vs. 0.54 ± 0.22 in CKD alone; P = 0.0087).
Conclusion(s)
These findings demonstrate that CKD is associated with early microglial activation and subsequent neuroinflammation in brain regions regulating sympathetic tone. This neuroimmune activation precedes and contributes to heightened SNA, independent of neurovascular dysfunction. Microglial depletion attenuates sympathetic overactivity, identifying microglia as a mechanistic driver of excess SNA in CKD and a potential therapeutic target.
More abstracts on this topic:
Heart-Brain Connection: White Matter Hyperintensity Associated with Low Heart Rate Variability
Martin Ansley, Parrish Michael, Suri Fareed, Rosamond Wayne, Wasserman Bruce, Sen Souvik
84 Immune checkpoint profiling in major aortic diseases leads to identification of potential roles of CD155-CD206 pathway in suppressing inflammation and immune responsesShao Ying, Saaoud Fatma, Xu Keman, Lu Yifan, Jiang Xiaohua, Wang Hong, Yang Xiaofeng