Final ID: FR405
Beyond Preeclampsia: Hypertension and Proteinuria in Pregnancy
Abstract Body: Case: A 35-year-old female with a history of migraines, bipolar disorder, anxiety, and presumed ‘white-coat hypertension’ presented at 10 weeks gestation to her obstetric visit with hypertension to 134/88, mildly elevated 24-hour urine protein (24hUP), and normal urine protein/creatinine ratio (UPCR). She was prescribed aspirin for preeclampsia risk reduction. Mild hypertension persisted through the pregnancy without symptoms. At 36 weeks gestation, she was hypertensive to 148/94 with headaches, chest pain, and lower extremity edema as well as significant proteinuria (24hUP and UPCR). She was diagnosed with preeclampsia and labor was induced at 37 weeks. After an uncomplicated delivery, she was discharged on nifedipine and labetalol, but remained hypertensive and edematous, prompting referral to our Hypertension Center. Despite initiation of enalapril, proteinuria worsened.
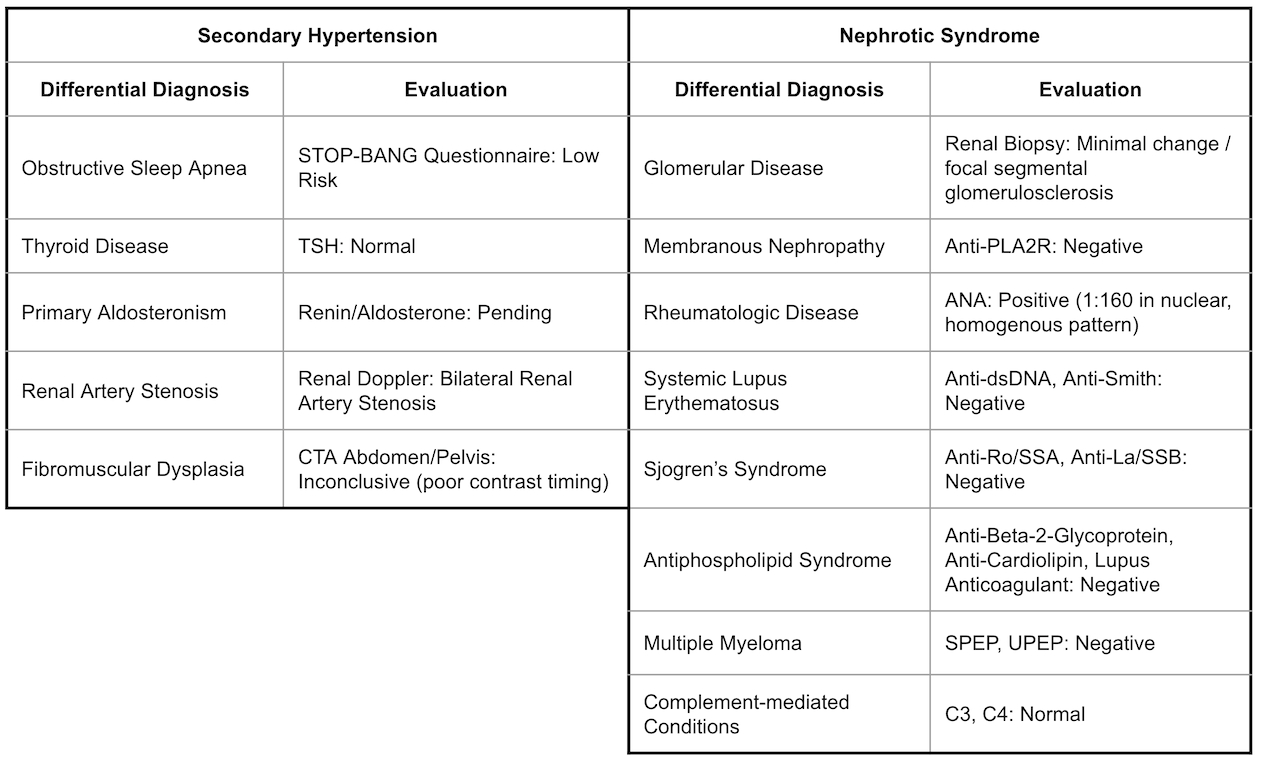
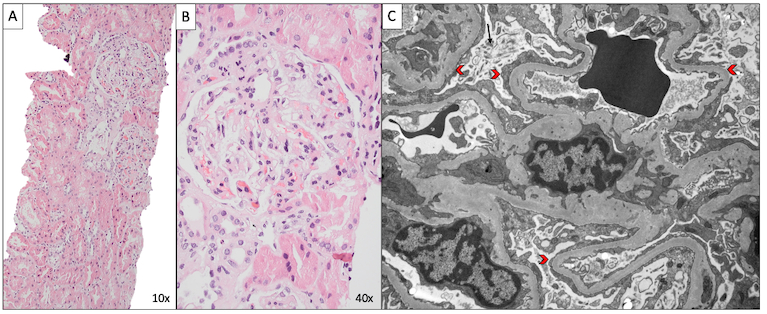
Differential Diagnosis: A broad differential was considered for her hypertension and proteinuria but ultimately her clinical picture was deemed most consistent with nephrotic syndrome superimposed on chronic hypertension (Fig 1). Renal biopsy showed minimal change disease/focal segmental glomerulosclerosis (MCD/FSGS) (Fig 2).
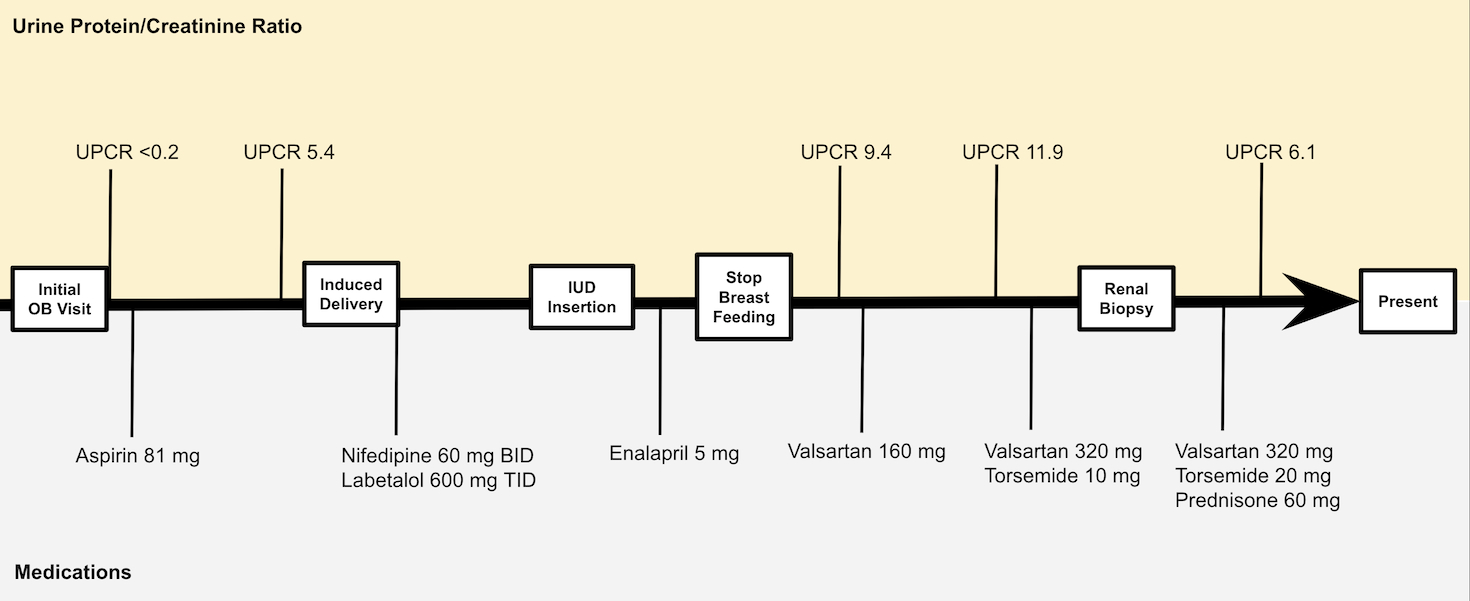
Treatment/Management: Medications were adjusted based on blood pressure and symptoms while her evaluation continued (Fig 3). Enalapril was transitioned to valsartan after she stopped breastfeeding. Torsemide was initiated to manage edema. After the renal biopsy results were known, she was started on prednisone.
Outcome: Currently her blood pressure is controlled and her UPCR is trending down.
Discussion: Chronic hypertension with superimposed preeclampsia is quite common, whereas de novo glomerular disease is rare. While hypertension may persist postpartum in those with preeclampsia, proteinuria tends to resolve within weeks. The worsening proteinuria over the ensuing months suggests a glomerular process unrelated to preeclampsia. Steroids are an effective and safe treatment in pregnancy; tacrolimus can be used in cases of steroid resistance or contraindication. Case reports of MCD in pregnancy describe a range of outcomes including spontaneous resolution, concomitant lupus nephritis, and progressive renal failure requiring intrapartum hemodialysis. Fetal complications include intrauterine growth restriction and fetal death. Fortunately, our patient’s renal function remained stable throughout her pregnancy and she delivered a newborn without complications.
Differential Diagnosis: A broad differential was considered for her hypertension and proteinuria but ultimately her clinical picture was deemed most consistent with nephrotic syndrome superimposed on chronic hypertension (Fig 1). Renal biopsy showed minimal change disease/focal segmental glomerulosclerosis (MCD/FSGS) (Fig 2).
Treatment/Management: Medications were adjusted based on blood pressure and symptoms while her evaluation continued (Fig 3). Enalapril was transitioned to valsartan after she stopped breastfeeding. Torsemide was initiated to manage edema. After the renal biopsy results were known, she was started on prednisone.
Outcome: Currently her blood pressure is controlled and her UPCR is trending down.
Discussion: Chronic hypertension with superimposed preeclampsia is quite common, whereas de novo glomerular disease is rare. While hypertension may persist postpartum in those with preeclampsia, proteinuria tends to resolve within weeks. The worsening proteinuria over the ensuing months suggests a glomerular process unrelated to preeclampsia. Steroids are an effective and safe treatment in pregnancy; tacrolimus can be used in cases of steroid resistance or contraindication. Case reports of MCD in pregnancy describe a range of outcomes including spontaneous resolution, concomitant lupus nephritis, and progressive renal failure requiring intrapartum hemodialysis. Fetal complications include intrauterine growth restriction and fetal death. Fortunately, our patient’s renal function remained stable throughout her pregnancy and she delivered a newborn without complications.
More abstracts on this topic:
A Blood(y) Pressure Crisis: Diffuse Alveolar Hemorrhage as a Rare Manifestation of Severely Uncontrolled Hypertension
Nandyal Shreyas, Amdetsion Gedion Yilma, Varma Revati, Kohli Saksham, Hammo Hasan
A major effect of aprocitentan on albuminuria in patients with resistant hypertensionSchlaich Markus, Bakris George, Flack John, Gimona Alberto, Narkiewicz Krzysztof, Sassi-sayadi Mouna, Wang Jiguang, Weber Michael