Final ID: TAC165
Nighttime Blood Pressure and Intracranial Atherosclerotic Stenosis: Dose-Response Associations With Atherosclerotic Burden and Symptomatic Status
Abstract Body: Background: Hypertension is a primary vascular risk factor for intracranial atherosclerotic stenosis (ICAS) and contributes to its progression. While existing studies have predominantly focused on static office blood pressure (BP) measurements, little is known about the relationship between ambulatory BP patterns and ICAS pathophysiology, which may inform a targeted preventive strategy.
Methods: In this multicenter observational study, 301 patients with ICAS underwent 24-hour ambulatory BP monitoring, magnetic resonance angiography (MRA), and high-resolution vessel wall imaging. We investigated the associations between ambulatory BP parameters and ICAS burden, stratified by the number of vessels exhibiting 50%-99% stenosis or occlusion, and symptomatic status (symptomatic ICAS or asymptomatic ICAS).
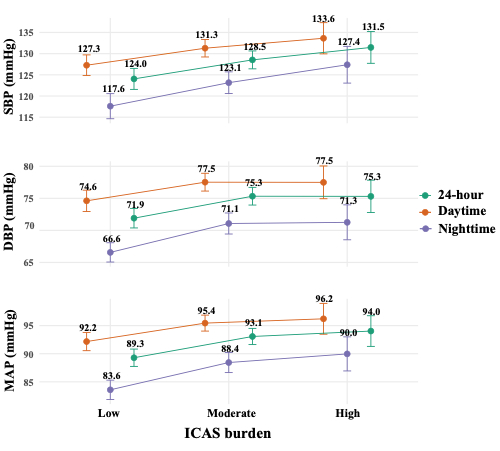
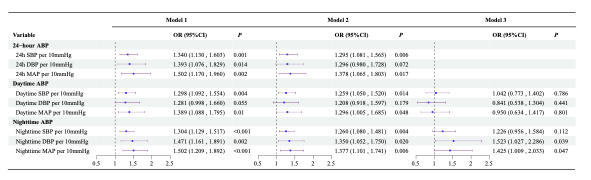
Results: In multivariable logistic regression models, after adjusting for traditional cardiovascular risk factors, both daytime and nighttime blood pressure were associated with ICAS burden and symptomatic status. However, only nighttime BP, but not daytime BP, remained an independent association after further mutual adjustment for daytime and nighttime blood pressure. Each 10 mmHg increase in nighttime systolic blood pressure (SBP), diastolic blood pressure (DBP) and mean arterial pressure (MAP), was associated with a 36.5%(95% CI 1.090-1.716), 50.9% (95% CI 1.065-2.149) and 51.2% (95% CI 1.111-2.067) increase in the odds of progressing to a higher grade of ICAS burden, respectively. Each 10 mmHg increase in nighttime DBP and nighttime MAP was associated with a 52.3% (95% CI 1.027–2.286) and 42.5% (95% CI 1.009–2.033) higher odds of symptomatic ICAS.
Conclusions: Nighttime BP showed independent dose-response associations with ICAS burden and symptomatic status, indicating its potential value in risk stratification. Prospective studies are needed to confirm its clinical utility.
Methods: In this multicenter observational study, 301 patients with ICAS underwent 24-hour ambulatory BP monitoring, magnetic resonance angiography (MRA), and high-resolution vessel wall imaging. We investigated the associations between ambulatory BP parameters and ICAS burden, stratified by the number of vessels exhibiting 50%-99% stenosis or occlusion, and symptomatic status (symptomatic ICAS or asymptomatic ICAS).
Results: In multivariable logistic regression models, after adjusting for traditional cardiovascular risk factors, both daytime and nighttime blood pressure were associated with ICAS burden and symptomatic status. However, only nighttime BP, but not daytime BP, remained an independent association after further mutual adjustment for daytime and nighttime blood pressure. Each 10 mmHg increase in nighttime systolic blood pressure (SBP), diastolic blood pressure (DBP) and mean arterial pressure (MAP), was associated with a 36.5%(95% CI 1.090-1.716), 50.9% (95% CI 1.065-2.149) and 51.2% (95% CI 1.111-2.067) increase in the odds of progressing to a higher grade of ICAS burden, respectively. Each 10 mmHg increase in nighttime DBP and nighttime MAP was associated with a 52.3% (95% CI 1.027–2.286) and 42.5% (95% CI 1.009–2.033) higher odds of symptomatic ICAS.
Conclusions: Nighttime BP showed independent dose-response associations with ICAS burden and symptomatic status, indicating its potential value in risk stratification. Prospective studies are needed to confirm its clinical utility.
More abstracts on this topic:
10-Year Trends in Last Known Well to Arrival Time in Acute Ischemic Stroke Patients: 2014-2023
Ferrone Nicholas, Sanmartin Maria, O'hara Joseph, Jimenez Jean, Ferrone Sophia, Wang Jason, Katz Jeffrey, Sanelli Pina
A Daily Diary Examination of the Associations of Adverse Childhood Experiences, Anticipated Discrimination, and Blood Pressure among Sexual and Gender Minority AdultsPardee Lisa, Bochicchio Lauren, Caceres Billy