Final ID: TH290
Blood Pressure Trajectory and Treatment Patterns Among Older Patients with Apparent Treatment Resistant Hypertension: Insights from a Large, Community-Based Healthcare System
Abstract Body: Background:
Aging increases the risk of resistant hypertension which is associated with an increased risk of mortality and cardiovascular events. Here, we examined the characteristics, blood pressure (BP) trajectories, and treatment patterns of older patients with apparent treatment resistant hypertension (aTRH).
Hypothesis:
We hypothesized aTRH would be undertreated, especially in octogenarians.
Methods:
We conducted a retrospective study of all patients with two available ambulatory BP measurements separated by at least 3 months in a community-based teaching hospital. aTRH was defined as BP above goal despite the use of ≥3 antihypertensive medication classes or controlled BP on ≥4 antihypertensive medication classes.
Results:
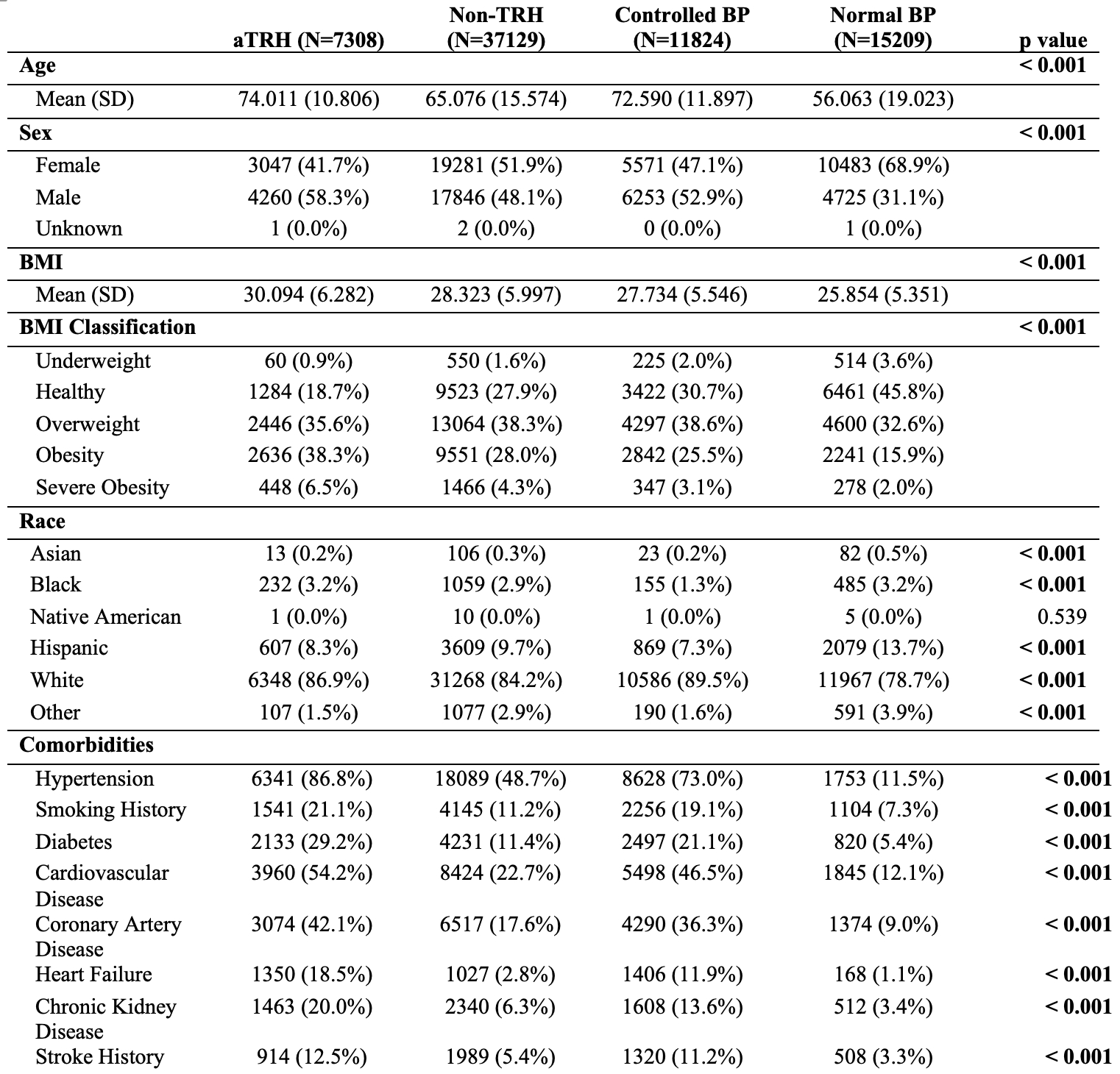
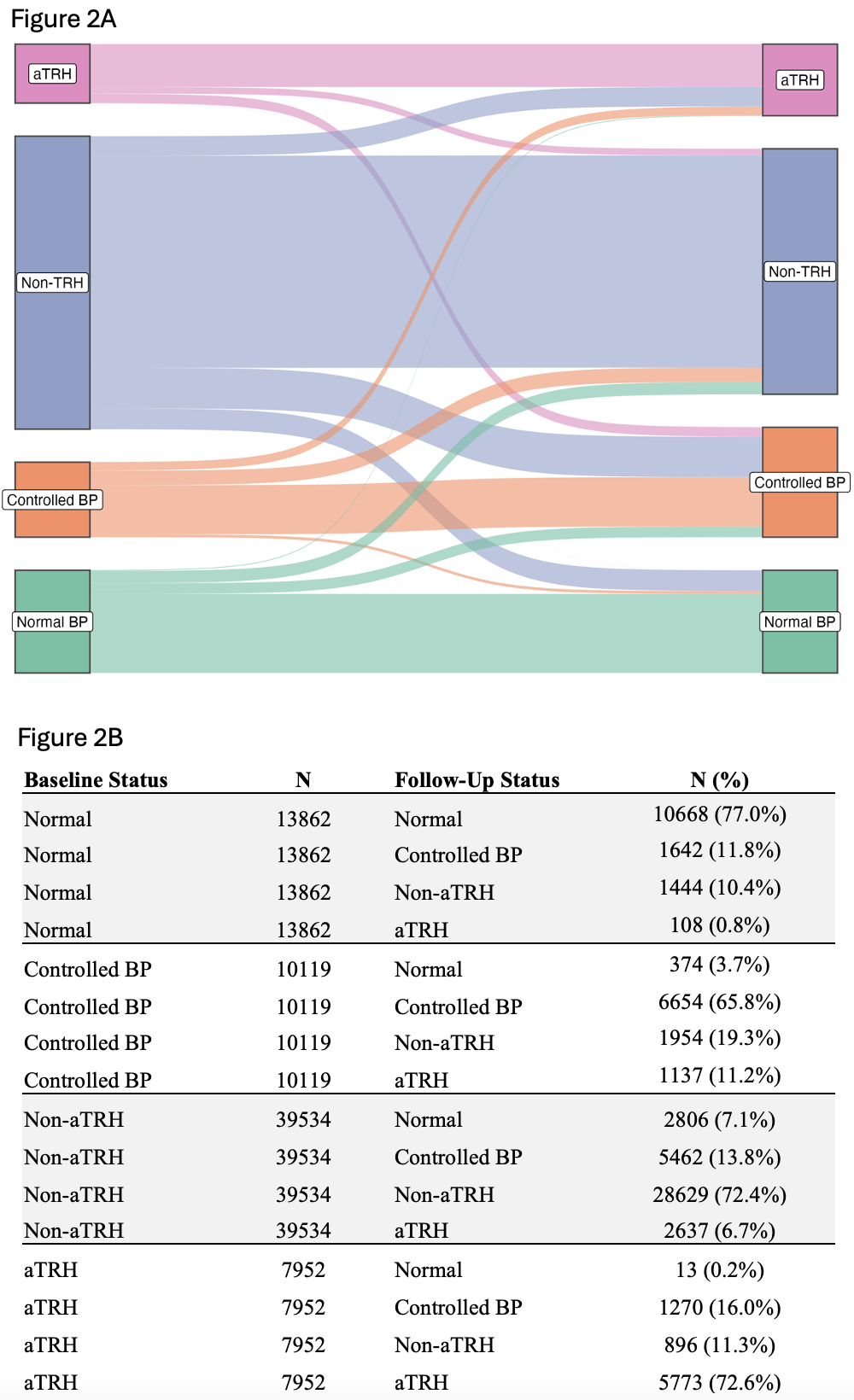
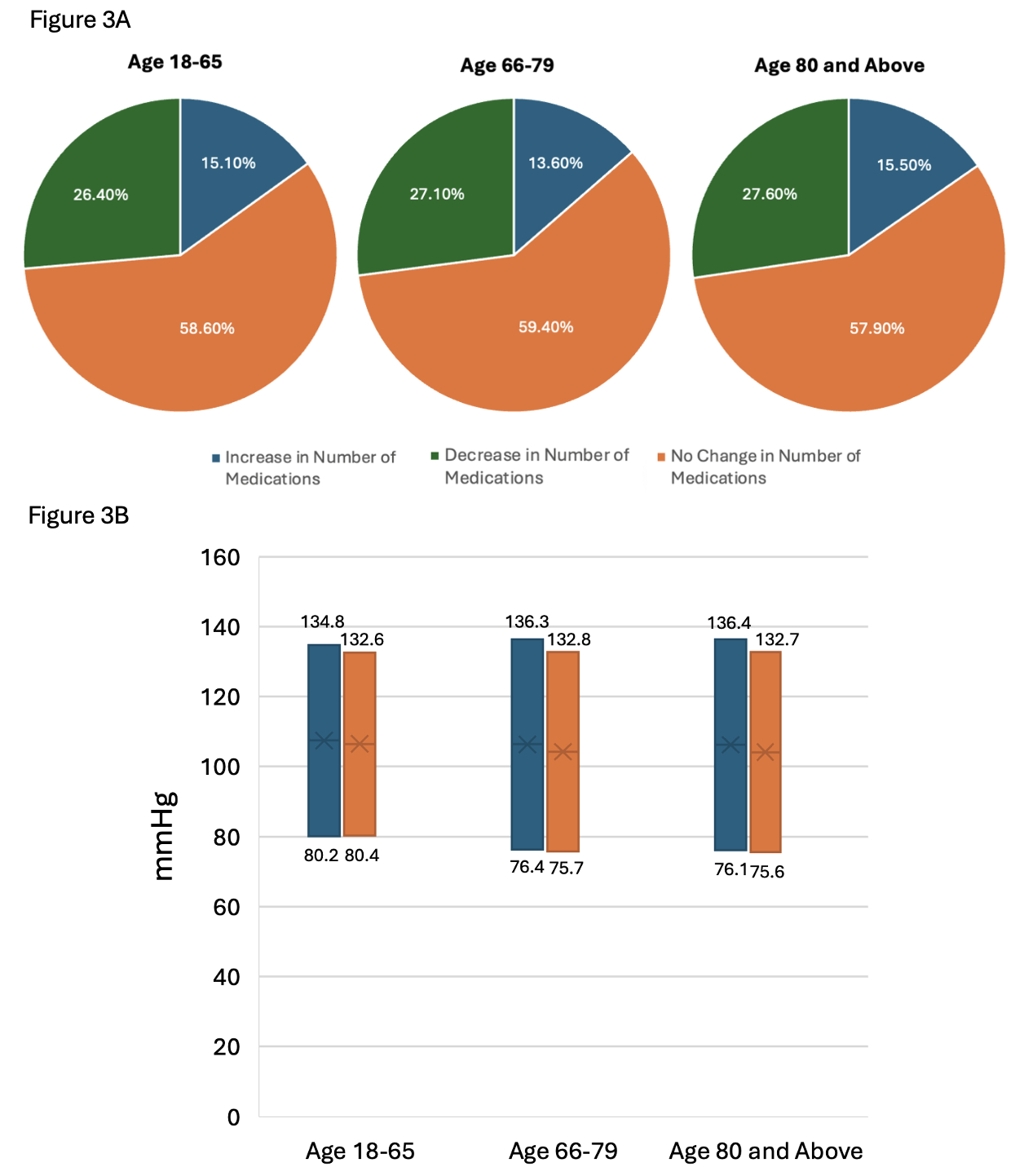
Of the 71,470 patients with available data, 7308 (10.2%) met criteria for aTRH with a mean follow-up length of 18.9 months. Compared to patients with normal BP, patients with aTRH were older with a mean age of 74 years versus 65 years (p<0.001). Patients with aTRH were more likely to be males (58.3%) compared to the normal BP groups (40.6%, p<0.001) (Figure 1). Compared to patients with normal BP, patients with aTRH were more likely to be obese and have a higher prevalence of smoking history, diabetes, coronary artery disease, heart failure, peripheral arterial disease, atrial fibrillation, and chronic kidney disease (Figure 1). Amongst those with aTRH, 1566 (5.3%) were aged 18-65, 3763 (13.2%) were aged 66-79, and 2623 (19.7%) were ≥80 years old. At follow-up, among those with aTRH at baseline, 5773 (72.6%) remained with aTRH, 896 (11.3%) improved to non-aTRH, 1270 (16.0%) improved to controlled BP, and 13 (0.2%) improved to normal BP (Figure 2). Most patients irrespective of age had no change in the number of medications at follow-up; only 15.5% of octogenarians with aTRH had an increase in antihypertensives (Figure 3). Between baseline and follow up, octogenarians as a whole had a systolic BP drop of -2.34 (p<0.001), and diastolic BP drop of -0.56 (p=0.061), whereas octogenarians with aTRH had a systolic BP drop of -3.7 (p<0.001) and diastolic BP drop of -0.55 (p=0.050).
Conclusion:
In an ambulatory population of patients at a community hospital, the prevalence of aTRH was high among patients ≥80 years and associated with established cardiovascular risk factors. Most patients with aTRH do not have a change in BP status over time. Anti-hypertensive medication escalation is infrequent among patients with aTRH irrespective of age.
Aging increases the risk of resistant hypertension which is associated with an increased risk of mortality and cardiovascular events. Here, we examined the characteristics, blood pressure (BP) trajectories, and treatment patterns of older patients with apparent treatment resistant hypertension (aTRH).
Hypothesis:
We hypothesized aTRH would be undertreated, especially in octogenarians.
Methods:
We conducted a retrospective study of all patients with two available ambulatory BP measurements separated by at least 3 months in a community-based teaching hospital. aTRH was defined as BP above goal despite the use of ≥3 antihypertensive medication classes or controlled BP on ≥4 antihypertensive medication classes.
Results:
Of the 71,470 patients with available data, 7308 (10.2%) met criteria for aTRH with a mean follow-up length of 18.9 months. Compared to patients with normal BP, patients with aTRH were older with a mean age of 74 years versus 65 years (p<0.001). Patients with aTRH were more likely to be males (58.3%) compared to the normal BP groups (40.6%, p<0.001) (Figure 1). Compared to patients with normal BP, patients with aTRH were more likely to be obese and have a higher prevalence of smoking history, diabetes, coronary artery disease, heart failure, peripheral arterial disease, atrial fibrillation, and chronic kidney disease (Figure 1). Amongst those with aTRH, 1566 (5.3%) were aged 18-65, 3763 (13.2%) were aged 66-79, and 2623 (19.7%) were ≥80 years old. At follow-up, among those with aTRH at baseline, 5773 (72.6%) remained with aTRH, 896 (11.3%) improved to non-aTRH, 1270 (16.0%) improved to controlled BP, and 13 (0.2%) improved to normal BP (Figure 2). Most patients irrespective of age had no change in the number of medications at follow-up; only 15.5% of octogenarians with aTRH had an increase in antihypertensives (Figure 3). Between baseline and follow up, octogenarians as a whole had a systolic BP drop of -2.34 (p<0.001), and diastolic BP drop of -0.56 (p=0.061), whereas octogenarians with aTRH had a systolic BP drop of -3.7 (p<0.001) and diastolic BP drop of -0.55 (p=0.050).
Conclusion:
In an ambulatory population of patients at a community hospital, the prevalence of aTRH was high among patients ≥80 years and associated with established cardiovascular risk factors. Most patients with aTRH do not have a change in BP status over time. Anti-hypertensive medication escalation is infrequent among patients with aTRH irrespective of age.
More abstracts on this topic:
Association of Delayed Diagnosis of Transthyretin Cardiomyopathy with Heart Failure Hospitalizations and Mortality
Spencer-bonilla Gabriela, Huang Joanna, Witteles Ronald, Heidenreich Paul, Sandhu Alexander, Alexander Kevin, Fan Jun, Cheng Paul, Din Natasha, Rodriguez Fatima, Varshney Anubodh, Davies Marie, Venditto John, Papas Mia
Improving In-Hospital Sleep Hygiene to Prevent and Curtail Delirium Among Older Adults: A Step-Wedge Cluster Randomized TrialVahidy Farhaan, Agarwal Katy, Nowakowski Sara, Bruce Courtenay, Potter Thomas, Pan Alan, Nair Rejani, Wenzlawsh Stephanie, Taffet George